An integrated approach to functional neurological disorder treatment can help to improve strength and mobility, reduce pain, and help people with the condition regain function and independence.
Functional neurological disorder or FND, is a condition that affects the central nervous system, resulting in symptoms such as weakness, seizures, tremors, balance problems, and difficulties with speech and memory.
In this article we will explore is the varying symptoms and presentation of FND, how it is diagnosed, and what risk factors can predispose an individual to develop it.
I will also discuss our integrated approach to functional neurological disorder treatment that may include physiotherapy, massage therapy, occupational therapy and exercise programming.
Table of Contents
- What is functional neurological disorder?
- Signs and symptoms of FND
- Diagnosing functional neurological disorder
- Causes and risk factors
- Functional neurological disorder treatment
- Client case study
- Conclusion
What is Functional Neurological Disorder?
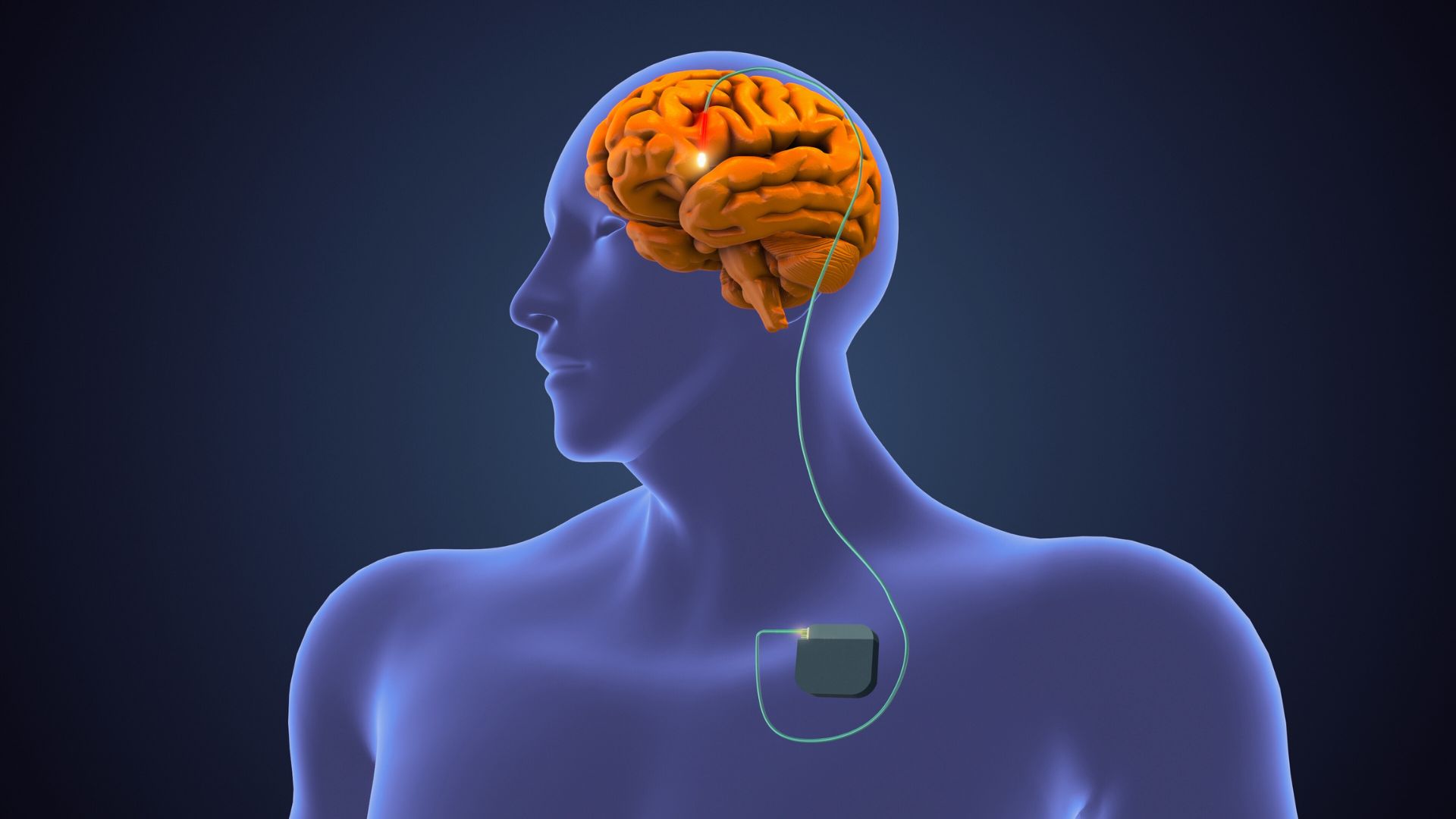
Functional neurological disorder is a medical condition that impacts the functioning of the brain. Specifically, the way the brain receives and sends information to the rest of the body is altered.
Although there is no known cause of FND, it often occurs following a recent psychological stressor that converts to physical signs and symptoms.[i]. These signs and symptoms, however, cannot be explained anatomically, and can vary from person to person.
Approximately 6% of neurology outpatients receive a diagnosis of FND and it is estimated 4-12 people per 100,000 will develop FND.[ii] While it can affect anyone of any age, it is uncommon in kids under 10 years old, and is more often found in women than in men.[iii]
Functional Neurological Disorder Symptoms and Signs
There are various signs and symptoms seen in individuals with FND. Some patients may only have a few of these symptoms while others have multiple symptoms.[iv]
These symptoms can include:
- Weakness: this most often occurs in the leg(s) or arm(s). This can result in difficulties with walking and standing, inability to hold objects, and the patient reporting “feeling the limb is not a part of them.” Sometimes the weakness can mimic a stroke, however, unlike a stroke, the tests will not reveal any structural problems to the brain.
- Seizures: this often looks like an epileptic seizure or fainting. It can present with uncontrolled shaking, suddenly going motionless and unresponsive and/or staring without responding to surroundings.
- Tremors: uncontrolled shaking of a body part (often the arms and/or legs)
- Involuntary twisting or jerking of a muscle of group of muscle: this usually occurs when someone is making sudden movements. With FND these are often more frequent.
- Problems with walking, posture and/or balance
- Muscle stiffness
- Speech and swallowing difficulties: this can present as slurred speech, stuttering, difficulty swallowing.
- Cognitive symptoms: memory and/or concentration can be a symptom of FND. Individuals may lose track of tasks they want to complete, go blank when doing a task or during a conversation, forget words, and misplace items such as their phone or keys. Many individuals without FND experience these however someone with FND will experience this frequently where it interferes with their ability to perform in their home and work life.
Diagnosing Functional Neurological Disorder
Functional neurological disorder often causes neurological symptoms without a structural problem occurring to the brain, and with no abnormal findings on diagnostic imaging such as MRIs, CT scans and blood.
FND is based on a clinical diagnosis often made by a neurologist, psychiatrist, or psychologist. They often look for a specific pattern of symptoms or signs in order to make the diagnosis.
Functional Neurological Disorder Causes and Risk Factors
The exact cause of FND is unknown and there are many different situations where these symptoms can start. In most occurrences, there is no known cause. In others, symptoms may come on after a head injury, an accident (e.g.: car accident), following surgery, following an infection like the flu virus, or following non-physical stressful event like divorce.[v]
There are many pre-disposing factors that may make some patients more susceptible to developing FND than others. Psychological disorders and stressful life events are believed to be risk factors for developing this condition but do not provide a full explanation and are not present in all patients presenting with FND.[vi]
Functional Neurological Disorder Treatment
Functional neurological disorder treatment often requires a multidisciplinary approach – which can include physiotherapy, occupational therapy, psychotherapy and medical management.
There is increasing evidence of the importance of including physiotherapy in the treatment of individuals with FND who present with limb muscle weakness. The aim of physiotherapy is to help retrain movement patterns, improve activity tolerance and prevent complications such as further muscle weakness and tightness.[vii]
Common physiotherapy interventions include:
- Graded exercise to improve activity tolerance.
- Desensitization strategies for individuals experiencing hypersensitivity to touch.
- Pain and fatigue management.
- Equipment recommendations to help with walking.
- Neuromuscular electrical stimulation to improve muscle patterning.
- Facilitation to help with movement and postural control.[viii]
Client Case of Functional Neurological Disorder
We will demonstrate how a multidisciplinary approach occurs through a case example of a former client at Propel Physiotherapy who we will call Jill.
Jill is 45-year-old woman whose symptoms first began following a motor vehicle collision. Initially she presented with physical symptoms that included headaches, pain in her neck and low back, weakness on the left side in her arms and legs, reduced balance, as well as difficulties with finding the right words when having a conversation. In addition to these physical symptoms and signs, she also reported an increase in anxiety following the accident.
Initially, Jill needed assistance to complete activities of daily living such as cooking, cleaning, and lifting. Her symptoms also impacted her ability to function at work resulting in her having to take a medical leave.
Due to the amount of pain Jill was in, physiotherapy focused mostly on passive treatment. This included passive range of motion (where the therapist moves the limb for the patient to help improve her range) and soft tissue release. She was also seeing a massage therapist to help address the pain and begin introducing movement to her body. Movements first involved passively stretching and then progressed to active stretching.
As the pain reduced and she gained more confidence in her ability to complete activities, Jill indicated she wanted to return to strengthening exercises. This would help her to achieve her goals of performing activities around the home with less assistance and to return to swimming, an activity she greatly enjoyed prior to her accident.
As Jill began to return to activities, she continued to see various practitioners to help her reach her goals. This included the following practitioners:
- A registered massage therapist to help address muscle stiffness.
- A physiotherapist to work on improving her mobility and developing a strengthening program she can implement at home. Physiotherapy also included challenging balance activities, cardiovascular exercise to improve her exercise tolerance, and relearning functional movement patterns like lifting objects. Physiotherapy strategies also include education on diagnosis and expectations, self-management strategies, factors that may trigger symptoms.
- An exercise physiologist to improve her strength and balance.
- A psychotherapist to address stress and anxiety and provide tools (such as breath work and meditation) to help manage these symptoms.
- A speech-language pathologist to help with word-finding.
- An occupational therapist to help improve her ability to complete activities of daily living such as cooking and cleaning which were limited due to the pain and muscle stiffness. This included making equipment recommendations to assist her in being able to complete these activities.
- A psychiatrist and physiatrist for ongoing monitoring and medical management.
It is important to note that Jill did not necessarily return to swimming as many laps as before. She began by doing aquafit and doing leisure swimming in the pool and slowly began doing a few laps at a time.
Conclusion
One of the common findings in patients with FND is they may not always return to doing the exact same activity exactly as before but instead find a new way of doing the activity.
It is important to remember every patient is different –the symptoms present differently for everyone and therefore the progress they make and the goals they set will be different.
As always, the most important person in the healthcare team is the client! Based on the patient’s presentation and personal goals, specific therapeutic short-term and long-term goals will be set in collaboration with their healthcare team.
At Propel Physiotherapy our integrated team of massage therapists, occupational therapists, exercise specialists and physiotherapists are trained and experienced in treating complex conditions such as FND. We will work in collaboration, to provide a comprehensive treatment intervention to support your goals!
Contact us if you have any questions about functional neurological disorder or how our therapists can help you get back to activities you enjoy.
References
[i] https://www.physio-pedia.com/Functional_Neurological_Disorder
[ii] https://www.frontiersin.org/articles/10.3389/fneur.2020.580267/full
[iii] https://www.ninds.nih.gov/health-information/disorders/functional-neurologic-disorder#:~:text=Anyone%20can%20develop%20FND.,per%20100%2C000%20will%20develop%20FND.
[iv] https://www.nhsinform.scot/illnesses-and-conditions/brain-nerves-and-spinal-cord/functional-neurological-disorder#:~:text=Functional%20neurological%20disorder%20(FND)%20describes,or%20structure%2C%20of%20the%20brain.
[v] https://fndhope.org/fnd-guide/
[vi] https://fndhope.org/fnd-guide/
[vii] https://www.mayoclinic.org/diseases-conditions/conversion-disorder/diagnosis-treatment/drc-20355202
Written by