After years of research and publicity around high-profile case of chronic traumatic encephalopathy (CTE), we are learning more about the impacts of repeated head injuries, especially as it relates to contact sports.
Athletes with a history of concussions are more likely to sustain additional concussions, which can result in cognitive decline, depression, and early degenerative change.[i] Repeated head injuries or concussion is associated with CTE.
As neurological rehabilitation professionals, we regularly work with young athletes who have sustained concussions. Clinically, we notice that recovery is more difficult and prolonged with the more concussions an individual has experienced. There is also a lower threshold for what causes a concussion after having repeated concussions, leading to lost game time and, often lost school time in this population.
In this article, we look at the symptoms and causes of CTE, as well as treatment options and guidelines around prevention. We also look at recommendations that could drastically reduce the instances of concussion in youth hockey players.
Table of Contents:
- What is CTE?
- Symptoms of CTE
- Causes of CTE
- Incidence of CTE
- Treatment of CTE
- Prevention of CTE
- Proposed Guidelines for Contact in Youth Hockey
- Conclusion
What is CTE?
Chronic Traumatic Encephalopathy (CTE) is a progressive brain disorder associated with repeated head injuries or concussions.[ii] The symptoms and consequences of CTE can have devastating effects on patients and their families.
Currently, the diagnosis of CTE can only be made post-mortem and can therefore present challenges for clinicians
Symptoms of CTE
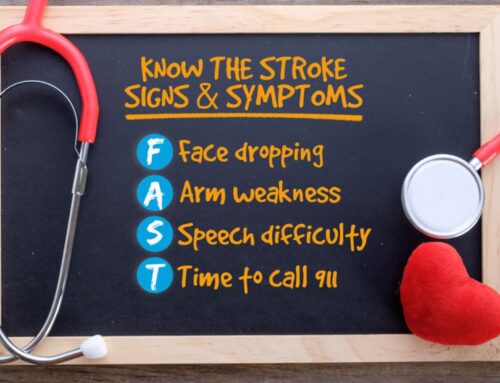
CTE symptoms often start gradually, approximately 10 years after repeated head injuries. Symptoms may get gradually worse after their onset, or they may plateau for a period of time before eventually getting worse.[iii]
- Symptoms include:[ii]
- Memory and thinking problems
- Confusion
- Personality changes
- Mood changes (depression, suicidal thoughts)
- Difficulties with balance and motor skills
- Cognitive difficulties such as decreased attention and difficulty organizing thoughts
Causes of CTE
CTE is caused by repeated blows to the head. It is more common in individuals who play contact sports, such as football, boxing, hockey, soccer, wrestling or rugby. It is also more commonly seen in military veterans.[ii]
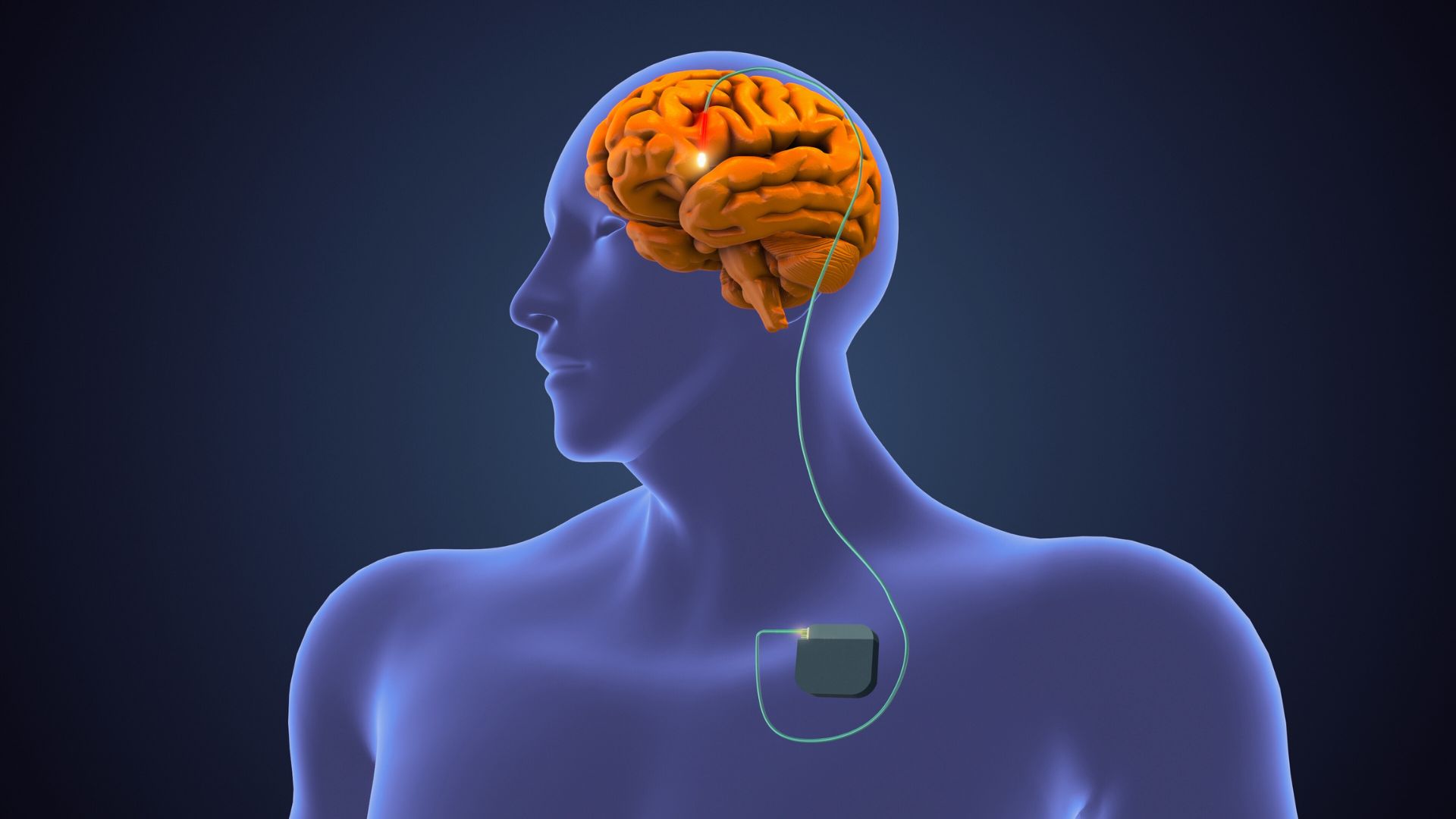
Similar to Alzheimers, CTE involves a buildup of tau protein in the brain. The pattern of buildup around the tissues and vessels in the brain is distinct from dementia and other brain diseases that involve the tau protein.[ii]
Incidence of CTE
The incidence of CTE is still unknown, particularly in young people. In a 2023 study in the JAMA Neurology, 152 brains (141 male and 11 female) were donated to a brain bank belonging to athletes who had sustained repetitive head injuries from playing contact sports and who died before the age of thirty. Of these brains, more than 40 percent were diagnosed with CTE, mostly in the mild stages.
The brains that were diagnosed with CTE tended to be older than those without signs of the disease, and the most common causes of death in both groups was suicide, followed by unintentional drug overdose.[iv]
This study found that 70 percent of the athletes who were diagnosed with CTE after their death played sports only at an amateur level. Three quarters of those affected played American football, followed by hockey, soccer, wresting, or rugby.
The football players who were diagnosed with CTE tended to play the sport longer than those who did not demonstrate signs of CTE.[iv] This study demonstrates that the signs of CTE in the brain may start earlier than previously thought.
CTE Treatment and Prevention
CTE is a progressive degenerative disease, and as such, there is no way to prevent its progression or reverse the course of the disease.[ii] Treatment for this population is focused on medical management for the cognitive and behavioural symptoms associated with the disease.
The current recommendation to prevent CTE is to reduce mild traumatic brain injuries and to prevent additional injury after a concussion. CTE can be prevented by avoiding blows to the head, particularly repeated blows to the head from contact sports.
Recently, there has been a call to increase the age at which bodychecking is permitted in youth hockey.
Proposed Guidelines for Contact in Youth Hockey
Typical concussions resolve in 7-10 days; however, there are several factors that can prolong recovery from a concussion and result in Post Concussion Syndrome (PCS). Symptoms of PCS can last from months to several years.
In 2022, Dr. Charles Tator, a neurosurgeon and leading expert at the Canadian Concussion Centre released a paper stating that “bodychecking was the commonest mechanism of prolonged disability from concussion in boys’ and girls’ hockey with average [post concussion syndrome] duration of 12.3 months but several years in some players”. Based on this, he has recommended that the age that bodychecking is permitted in hockey leagues be raised from 13-14 years old to 18 years old.[v]
In this case series, 87 hockey players, aged 10-18 years old were followed. Of these players, 70 individuals developed post-concussion syndrome (80.4 percent) and symptoms lasted 1-168 months in males and 3-26 months in females. Bodychecking was the most common cause of concussion in these players and caused post-concussion syndrome in 70.6 percent of cases.[v]
In this study, changing the bodychecking guidelines would have prevented the majority of bodycheck concussions that were sustained and prevented years of suffering from post-concussion syndrome.[v]
A recent position statement published by Dr. Kristian Goulet at the University of Ottawa, found that eliminating bodychecking could decrease rates of concussion in Canada from 20 – 90 percent in all age groups.[vi] This review advocates for delaying contact in hockey until a minimum age of 15, based on their review of the medical literature.
Policy changes like these will be instrumental in preventing post-concussion syndrome and chronic traumatic encephalopathy in amateur athletes in the future.
Conclusion
The clinical team at Propel Physiotherapy has extensive experience treating acute concussions as well as post-concussion syndrome from a variety of sources including sports injuries, slip and falls, and motor vehicle collisions.
We use best practice guidelines for management of post-concussion related symptoms and return to activity or sport. Once a diagnosis is made by a medical professional — sport medicine doctor, family doctor, neurologist, physiatrist — we work in collaboration to achieve an optimal outcome.
If you have any questions about concussion rehabilitation, or post-concussion syndrome, please reach out to us at info@propelphysiotherapy.com to schedule a complimentary consultation with one of our clinicians.
References
[i] Indharty RS, Siahaan AMP, Rosarina, Susanto M, Tandean S, Risfandi M. Prevention of sports-related concussion in soccer: a comprehensive review of the literature. Ann Med Surg (Lond). 2023 Mar 24;85(3):365-373. doi: 10.1097/MS9.0000000000000268. PMID: 37008175; PMCID: PMC10060082.
[ii] Chronic Traumatic Encephalopathy (CTE), Alzheimers Association
[iii] National Health Service, UK, Chronic Traumatic Encephalopathy
[iv] National Institutes of Health, Chronic traumatic encephalopathy in young athletes
[v] Tator CH, Blanchet V, Ma J. Persisting Concussion Symptoms from Bodychecking: Unrecognized Toll in Boys’ Ice Hockey. Canadian Journal of Neurological Sciences / Journal Canadien des Sciences Neurologiques. 2023;50(5):694-702. doi:10.1017/cjn.2022.289
[vi] Kristian Goulet, Suzanne Beno, Sport-related concussion and bodychecking in children and youth: Evaluation, management, and policy implications, Paediatrics & Child Health, Volume 28, Issue 4, July 2023, Pages 252–258, doi.org/10.1093/pch/pxad007
Written by