Deep brain stimulation Parkinson’s disease therapy has emerged as a promising option to offer relief to people who have not responded adequately to medication.[i] While deep brain stimulation (DBS) can effectively manage motor symptoms, there are limits to what it can do.
In this article, we take a closer look at how deep brain stimulation can be used to treat Parkinson’s disease symptoms and how to determine whether it is a fit for you. We also discuss the crucial role physiotherapy plays in maximizing recovery and improving overall quality of life for clients with Parkinson’s Disease post-surgery.
Table of Contents:
- What is Parkinson’s disease?
- What is deep brain stimulation Parkinson’s disease therapy?
- Is deep brain stimulation right for me?
- Challenges post-deep brain stimulation therapy
- Physiotherapy after deep brain stimulation
- Conclusion
What is Parkinson’s Disease (PD)?
Parkinson’s Disease (PD) is a progressive neurodegenerative disorder that affects the dopamine producing cells in the brain. Dopamine is a neurotransmitter that is needed to send signals between neurons to coordinate movement.
As a result, PD is characterized by motor symptoms such as tremors, slow movements, stiffness, balance difficulties and muscle cramping. Clients with PD may also experience non-motor symptoms such as depression, anxiety, fatigue and sleep issues, to name a few.
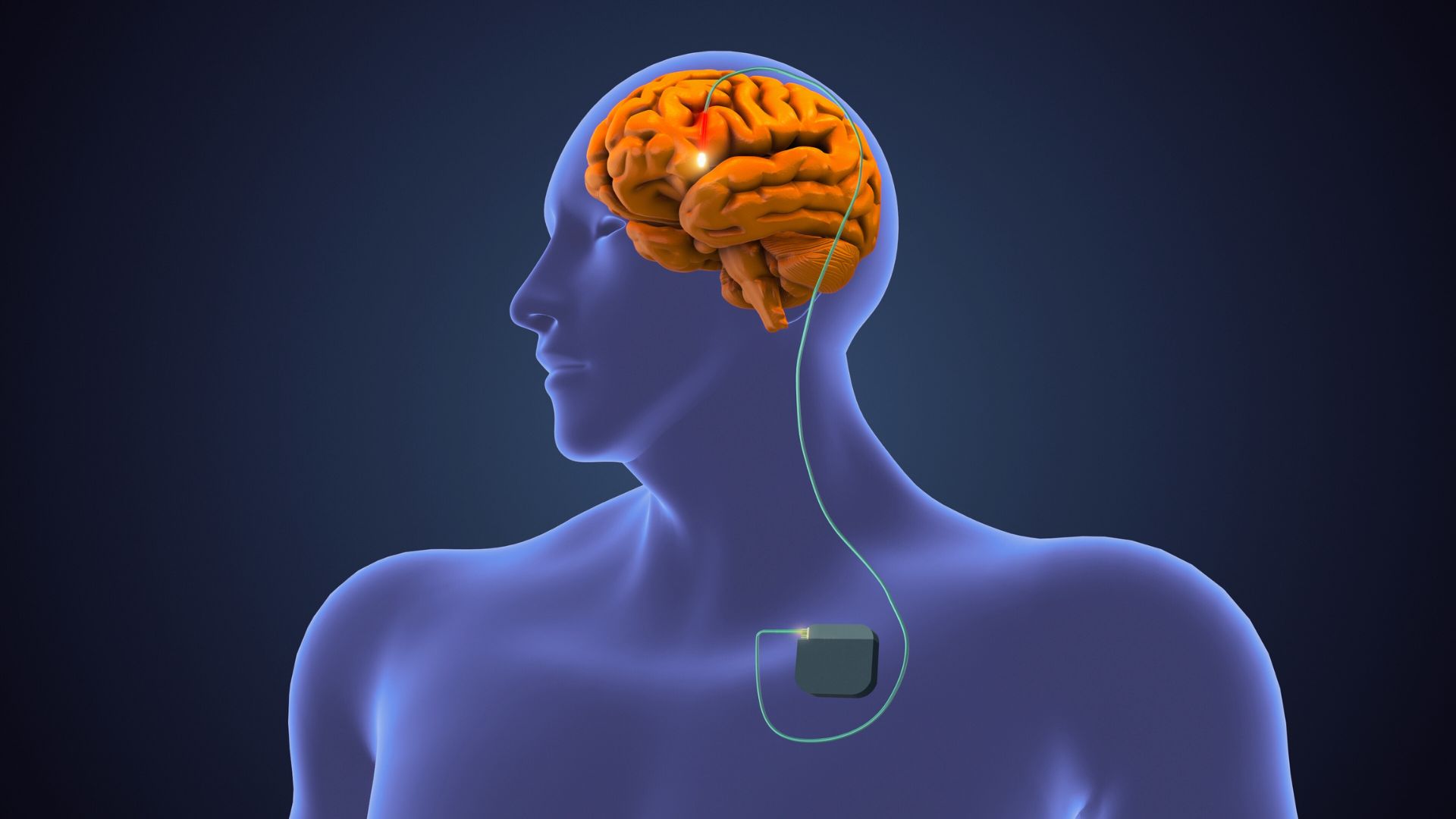
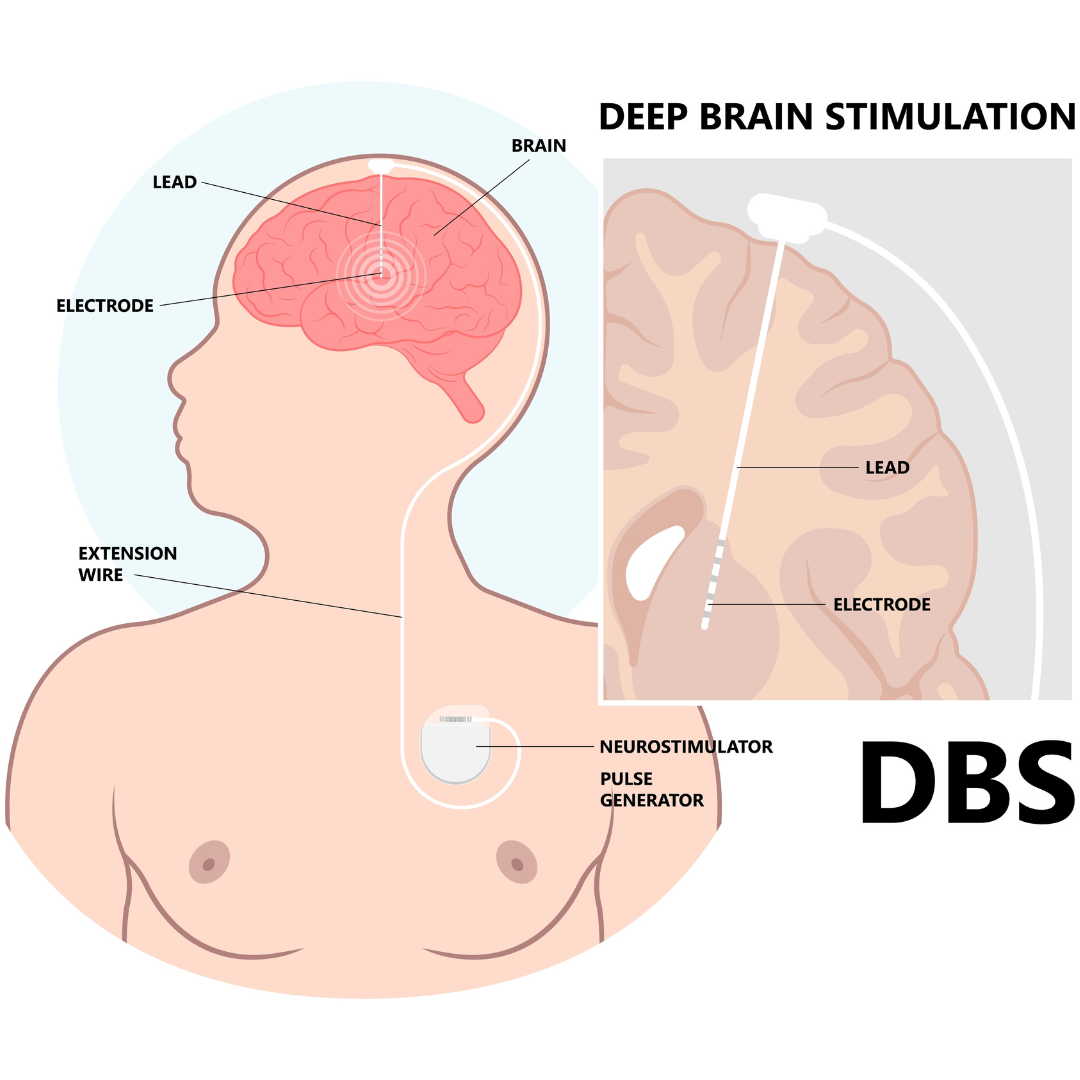
What is Deep Brain Stimulation Parkinson’s Disease Therapy
DBS is a surgical therapy that is used as a treatment for Parkinson’s Disease (PD). During the surgery a wire (referred to as a lead) is inserted into an area deep in the brain called the substantia nigra pars compacta (SNc). At this site, there are over 400,000 dopamine producing cells. The lead then delivers an electrical current to areas of the brain that are responsible for movement.
As a result, abnormal brain activity can be regulated which could lead to a reduction in symptoms of PD. Deep brain stimulation Parkinson’s disease therapy can be used to treat a number of motor symptoms associated with the disease including the following:
- Tremors
- Stiffness
- Bradykinesia (slowness of movement)
- Dystonia (persistent muscle contraction causing unwanted movements)
- DBS may also be helpful in areas of sleep, pain and urinary issues in PD.[ii]
Is Deep Brain Stimulation Parkinson’s Disease Therapy Right for Me?
In order to determine whether deep brain stimulation Parkinson’s disease therapy is the right fit for you, it is important to consult with your healthcare team which may include doctors, neurologists, neurosurgeons, neuropsychologists, movement disorder specialists and rehab specialists.
More generally, the following characteristics may indicate if you could potentially benefit from deep brain stimulation Parkinson’s disease therapy:
- A PD type that responds to levodopa.
- “On/off” fluctuations (motor and non-motor symptoms occur, stop and reoccur)
- Tremor that has not responded to medications.
- A history of trying various medications and treatments without desired success.
- PD symptoms that interfere with day-to-day activities.[iii]
Challenges Post-Deep Brain Stimulation Parkinson’s Disease Therapy
While deep brain stimulation Parkinson’s disease therapy can significantly improve motor symptoms, clients may still experience residual symptoms and functional limitations post-surgery. Additionally, the surgical procedure itself can lead to temporary impairments, such as weakness, balance disturbances, and difficulty with fine motor control.
Physiotherapy plays a crucial role in addressing these challenges and facilitating optimal recovery following DBS.
Physiotherapy After Deep Brain Stimulation Parkinson’s Disease Therapy
Physiotherapy can play a vital role in symptom management for clients that have undergone deep brain stimulation Parkinson’s disease therapy. Treatment methods and outcomes have been illustrated in various research studies, some of which will be discussed in the following section.
A review of scientific literature reveals that rehabilitation following DBS can improve daily living, reduce the dosage of medication needed to manage symptoms, improve balance, increase mobility and improve gait (walking).
Neurorehabilitation Following Surgery
A research study was conducted on patients in a hospital setting following DBS surgery. On average, patients began rehabilitation 20 days after surgery and remained in the facility for close to a month. During this time, stimulation parameters were changed approximately seven times per patient which highlights the importance of DBS programming following implantation.
As a result of receiving this early rehabilitation, patients improved in activities of daily living and were able to reduce their dose of levodopa medication by a considerable amount. This allowed the patients to become more independent before being discharged from hospital.[iv] Not only is rehabilitation important in promoting independence but it is also essential in improving balance and mobility.
Muscle Strengthening, Balance Training and Gait Training
In another study, participants underwent muscle strengthening and stretching, balance training and gait training for 40 minutes during a two-week period under the supervision of an experienced physiotherapist. Various tests were conducted including the Mini-Balance Evaluation Systems Test and Timed Up and Go Test which measure balance and mobility respectively.
Both balance and mobility significantly improved among participants between the beginning and end of the study. Similar to the neurorehabilitation study mentioned in the previous section, participants were also able to reduce their daily dose of levodopa significantly.[v]
Treadmill Training
Furthermore, another study evaluated how rhythmic auditory stimulation (RAS) assisted treadmill training and physiotherapy could improve the gait or walking pattern of clients. RAS is a therapeutic technique that involves using music or beats to help cue a more normal walking pattern.
Each treadmill training session lasted 30 minutes while physiotherapy sessions lasted 60 minutes and included exercises to help with flexibility, balance, agit and muscle strength. Study participants that were treated with DBS and physiotherapy/gait training increased their walking speed, performance and self-confidence compared to those with only physiotherapy and no DBS.
In addition, those that received physiotherapy/gait training combined with DBS improved in other areas such as memory, language and attention.[vi]
Conclusion
Physiotherapy plays a vital role for clients recovering from deep brain stimulation Parkinson’s disease therapy. helping to improve daily living, reduce the dosage of medication needed to manage symptoms, improve balance, increase mobility and walking.
Through a holistic approach encompassing rehabilitation exercises, gait training, range of motion exercises, coordination training, and client education, physiotherapists empower individuals to optimize their recovery and regain independence.
As an integral component of multidisciplinary care, physiotherapy continues to be a cornerstone in the management of Parkinson’s Disease, offering hope and support to clients on their journey towards improved health and well-being.
References
[i] Okun, M. S., Ramirez-Zamora, A., Zeilman, P. R., Barabas, M., Fasano, A., Fung, W. K., & Tarakad, A. (2023). Surgical Options: A Treatment Guide to Parksinson’s Disease. Parkinson’s Foundation.
[ii] Okun, M. S., Ramirez-Zamora, A., Zeilman, P. R., Barabas, M., Fasano, A., Fung, W. K., & Tarakad, A. (2023). Surgical Options: A Treatment Guide to Parksinson’s Disease. Parkinson’s Foundation.
[iii] Okun, M. S., Ramirez-Zamora, A., Zeilman, P. R., Barabas, M., Fasano, A., Fung, W. K., & Tarakad, A. (2023). Surgical Options: A Treatment Guide to Parksinson’s Disease. Parkinson’s Foundation.
[iv] Allert, N., Cheeran, B., Deuschl, G., Barbe, M. T., Csoti, I., Ebke, M., Glaser, M., Kang, J.-S., Kelm, S., Krack, P., Kroth, J., Jobst, U., Markus Leisse, Oliviero, A., Nolte , P. N., Quick-Weller, J., Strothjohann, M., Tamás, G., Werner, M., … Groppa, S. (2018). Postoperative rehabilitation after deep brain stimulation surgery for movement disorders. Clin Neurophysiol., 129(3), 592–601.
[v] Sato, K., Aita, N., Hokari, Y., Kitahara, E., Tani, M., Izawa, N., Hatori, K., Nakamura, R., Sasaki, F., Sekimoto, S., Jo, T., Oyama, G., Hatano, T., Shimo, Y., Iwamuro, H., Umemura, A., Hattori, N., & Fujiwara, T. (2019). Balance and gait improvements of postoperative rehabilitation in patients with parkinson’s disease treated with subthalamic nucleus deep brain stimulation (STN-DBS). Parkinson’s Disease, 2019, 1–5.
[vi] Naro, A., Pignolo, L., Sorbera, C., Latella, D., Billeri, L., Manuli, A., Portaro, S., Bruschetta, D., & Calabrò, R. S. (2020). A case-controlled pilot study on rhythmic auditory stimulation-assisted gait training and conventional physiotherapy in patients with Parkinson’s disease submitted to deep brain stimulation. Frontiers in Neurology, 11.
Written by