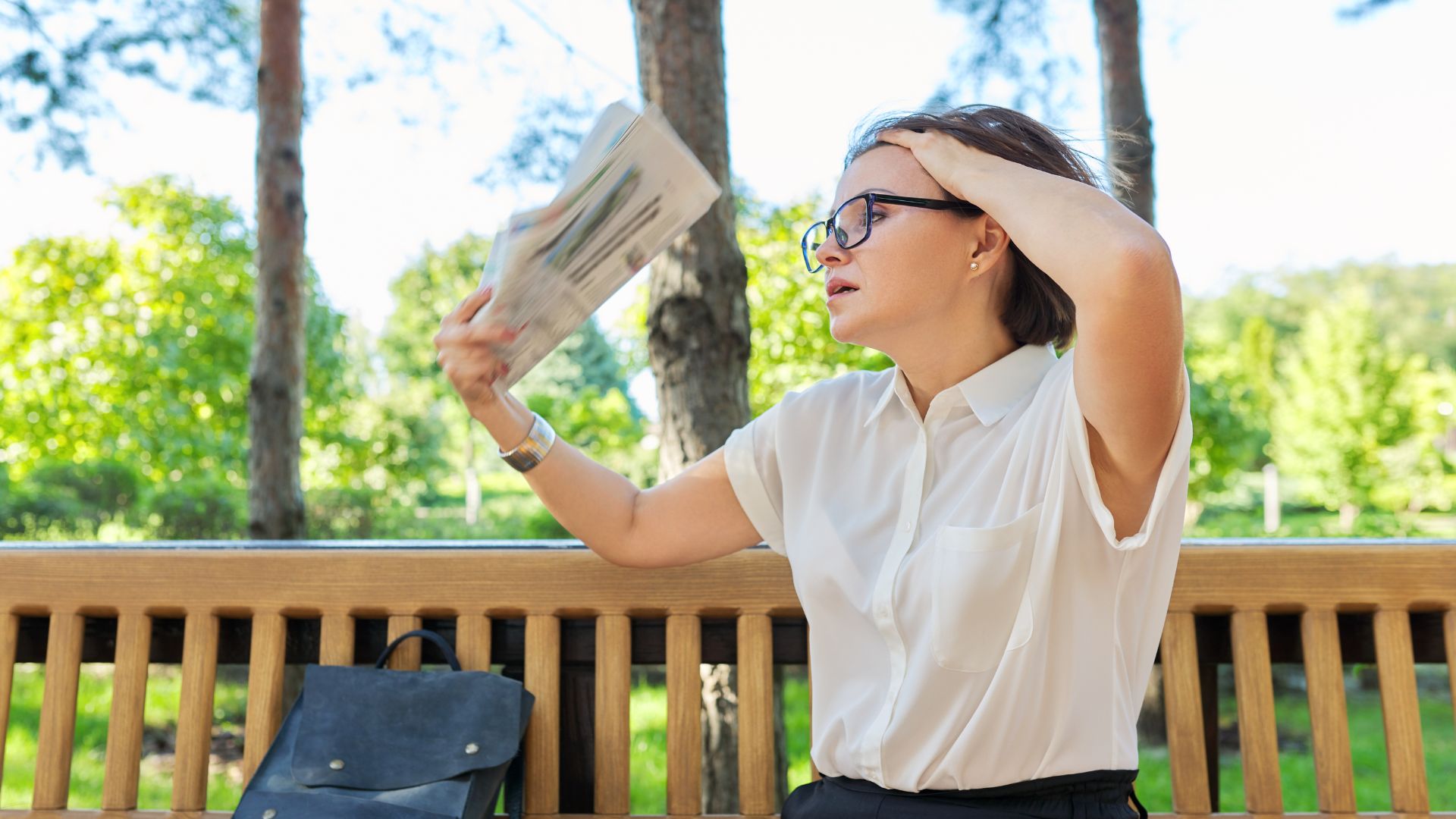
Menopause is a normal part of aging for women and can involve physical and emotional changes. The changing hormone levels that occur during menopause can result in a host of symptoms including hot flashes, mood changes, changes in body composition, decreased libido and changes in vaginal and vulvar tissues.
Lifestyle modifications can play a significant role in managing menopausal symptoms. In this article, we hear from four health professionals about the role of exercise, mindfulness, nutrition and pelvic physiotherapy in the management of menopause symptoms.
Table of Contents:
- How EXERCISE can help manage menopause symptoms
- Using MINDFULNESS to manage menopause symptoms
- PELVIC PHYSIOTHERAPY in managing menopause symptoms
- Management of menopausal symptoms with NUTRITION
- Menopause symptoms management conclusion
How Exercise Can Help Manage Menopause Symptoms
Regular exercise delivers physical and emotional benefits to women dealing with menopause. It can help reduce and prevent the negative effects of these hormonal changes during and post menopause by doing the following:
- Reducing stress
- Reducing heart disease and stroke
- Lowering high blood pressure and cholesterol
- Lowers risk of Type 2 diabetes by making your muscles more insulin sensitive
- Maintains bone health and lowers risk of Osteoporosis
- Controlling weight gain
- Building muscle strength by increasing metabolism
The Canadian Physical Activity guidelines suggest that for optimal health benefits, individuals 18-64 years of age should accumulate 150 minutes of moderate activity a week in bouts of 10 minutes or more. Strength training should be performed at least 2 times per week and older adults (>65 years) should add activities to enhance their balance.
Clinical Exercise Physiologist Martha Garrick says that building your overall fitness and strength is something that should be done as you would build your retirement. “The effects of menopause can sometimes be damaging but taking preventative measures is important. Health is wealth, and since 1/3 of woman’s life is spent in post menopause it is never too late to start being active,” says Garrick.
You may also enjoy reading: How Exercise Supports Brain Function During Menopause
Using Mindfulness to Manage Menopause Symptoms
Mindfulness, which is the practice of being fully present and engaged in the current moment without judgment, can be beneficial during menopause helping with:
- Stress Reduction: Menopause can be a stressful time for many women, as they navigate physical symptoms like hot flashes, mood swings, and sleep disturbances. Mindfulness techniques, such as deep breathing and meditation, can help reduce stress and promote relaxation.
- Emotional Well-being: Hormonal fluctuations during menopause can contribute to mood swings, irritability, and anxiety. Mindfulness practices encourage self-awareness and emotional regulation, helping women better manage their emotions and respond to situations with greater calmness.
- Improved Sleep: Sleep disturbances are common during menopause. Mindfulness-based techniques, such as mindful breathing or body scan meditations, can be effective in promoting relaxation and improving sleep quality.
- Coping with Uncertainty: Menopause is a significant life transition, and it can bring about feelings of uncertainty and loss. Mindfulness encourages acceptance and a non-judgmental attitude, which can be valuable in navigating the changes and embracing this new phase of life.
- Increased Self-Compassion: Menopause is a unique experience for each woman, and practicing self-compassion through mindfulness can help women be kinder to themselves as they navigate the challenges and changes associated with this life stage.
Mindfulness trainer Kathy Mileski says it is important to note that mindfulness is a skill that develops over time with regular practice. Additionally, participating in mindfulness-based programs or seeking guidance from trained professionals can offer more structured support.
You may also enjoy reading: Mindful Aging: The Benefits of Mindfulness Training for Older Adults
Pelvic Physiotherapy in Managing Menopause Symptoms
As women transition through menopause, they often encounter a variety of symptoms that can significantly impact their quality of life. One common yet frequently overlooked aspect is genitourinary syndrome of menopause (GUSM), affecting the vagina, vulva and bladder.
Understanding Genitourinary Syndrome of Menopause (GUSM)
GUSM encompasses a variety of symptoms which ultimately result from a decrease in estrogen and other sex hormones. Changes can occur to the labia majora/minora, clitoris, vestibule (vaginal opening), vaginal canal, urethra and the bladder.
Unlike the outdated term “vaginal atrophy,” GUSM acknowledges both physical changes and associated symptoms.
GUSM Physical Signs and Physiological Changes
The physical signs and physiological changes of GUSM include:
- Thinning of vulvar and vaginal tissues
- Thinning of labia majora/ minora
- Narrowing of the vaginal opening
- Decreased vaginal blood flow
- Decreased lubrication
- Reduced elasticity of the vaginal walls
- Increased vaginal pH as well as decreased vaginal flora
Recognizing GUSM Symptoms
The above physical signs and physiological changes may result in the following symptoms:
- Vaginal dryness
- Fissuring or cracking of vaginal tissues
- Vaginal itching, burning or “sandpaper-like” feeling
- Pain with intercourse and or bleeding after intercourse
- Decreased libido, impaired arousal/ orgasm function
- Urinary symptoms including urgency, increased frequency, incontinence
- Pelvic organ prolapse
- Increased frequency of urinary tract infections or bladder infections
GUSM Management Strategies
If left untreated, GUSM often does not improve and may be considered a chronic condition. Addressing GUSM requires a multifaceted approach aimed at alleviating symptoms and improving overall pelvic health.
Consulting your medical practitioner is crucial to determine if topical or systemic hormone therapy is recommended for you, as well as considering other forms of medical management.
Other important management strategies include:
- Vulvar Care: Gentle cleansing and moisturizing can help maintain vulvar health
- and minimize discomfort.Soap can be drying and irritating and should be avoided on vaginal and vulvar tissues.
- Lubrication: Using high-quality lubricants can help alleviate dryness and enhance comfort during sexual activity. Often a silicone based lubricant can be helpful for those experiencing symptoms of GUSM.
- Vaginal Moisturizers: Regular application of vaginal moisturizer may help restore moisture and elasticity to vaginal tissues. Look for products that are unscented.
- Pelvic Floor Assessment and Treatment: Pelvic floor physiotherapists play a crucial role in assessing pelvic floor function and providing individualized treatment. Through personalized assessment and treatment by a pelvic health physiotherapist, women are empowered with knowledge and tools to effectively manage their symptoms.
Pelvic health practitioner Christine Davies says that key interventions may include:
- Education on anatomy and physiology
- Addressing/ discussing lifestyle factors
- Bladder retraining to improve urinary symptoms
- Strengthening and/or relaxation exercises of the muscles of the pelvic floor
- Manual techniques for tissue relaxation
- Guidance on progressive stretching
- Guidance on the use of dilators
You may also enjoy reading: Pelvic Floor Exercises for Incontinence
Management of Menopausal Symptoms with Nutrition
Nutrition can aid in alleviating the challenges of menopause including weight gain, hot flashes and mood changes. Here are five key nutrition tips from nutritionist Kylie James to help manage menopausal symptoms effectively:
- Incorporate Healthy Fats: Despite concerns about weight gain, including healthy fats like omega-3 fatty acids from sources such as salmon, mackerel, chia seeds, flaxseeds, and hemp seeds can potentially reduce the frequency and severity of night sweats.
- Embrace Phytoestrogens: Phytoestrogens, found in soybeans, chickpeas, berries, flaxseeds, and grapes, mimic estrogen’s effects in the body. Incorporating these plant-based compounds into your diet may help manage symptoms by compensating for declining estrogen levels.
- Prioritize Fruits and Vegetables: Rich in vitamins, minerals, antioxidants, and fiber, fruits and vegetables support overall health and can alleviate menopausal symptoms. Research suggests that increasing intake, as seen in studies like the Women’s Health Initiative Dietary Modification trial, correlates with weight loss and reduced hot flashes.
- Ensure Adequate Protein Intake: As estrogen levels decline during menopause, maintaining muscle mass and bone density becomes crucial. Consuming protein from sources such as eggs, lean meats, fish, and plant-based options like beans and lentils supports muscle and bone health, potentially mitigating symptoms.
- Limit Refined Sugar: Avoiding refined sugars, known for causing blood sugar spikes and mood swings, is particularly important for menopausal women. High sugar intake has been associated with increased incidence of depression and worsened menopausal symptoms like hot flashes and night sweats.
By following these five dietary recommendations, women experiencing menopausal symptoms can better manage their health and well-being, allowing them to focus on enjoying life to the fullest.
You may also enjoy reading: Exercise and Menopause: Effects on Body Composition, Bone Density & Mood
Menopause Symptoms Management Conclusion
Managing menopausal symptoms involves a holistic approach addressing physical, emotional and lifestyle issues, including referrals for medical interventions to optimize symptom management when necessary. While the symptoms of menopause can be challenging, there are many factors and steps that women can take to manage their symptoms.
References
- Haff, G., & Triplett, N. T. (2016). Essentials of strength training and conditioning. Fourth edition. Champaign, IL, Human Kinetics.
- Ball, Derek. “Metabolic and endocrine response to exercise: sympathoadrenal integration with skeletal muscle.” Journal of Endocrinology224.2 (2015): R79-R95
- Payne, JM (2021, Feb, 18) Why You Should Exercise Your Way Through Menopause. Lancastergeneralhealth.org
- Friedenreich, Christine M., et al. “Effects of a high vs moderate volume of aerobic exercise on adiposity outcomes in postmenopausal women: a randomized clinical trial.” JAMA oncology1.6 (2015): 766-776.
- Stojanovska, Lily, et al. “To exercise, or, not to exercise, during menopause and beyond.” Maturitas77.4 (2014): 318-323.
- MenopauseandU.ca Exercise and an active lifestyle
- Canadian Physical Activity Guidelines for Adults 18-64 years, CSEP.ca
- Canadian Physical Activity Guidelines for Older Adults 65 years & older, CSEP.ca
Written by