Loss of bladder control resulting in involuntary leakage of urine is fairly common. In fact, it is so common that many individuals do not discuss their symptoms with their doctor and are not aware that urinary incontinence treatment is available.
There are many factors that can increase one’s risk of urinary incontinence. However, in no situation should it be accepted as normal or simply tolerated. In this article, we will discuss the two most common types of urinary incontinence and how pelvic floor physiotherapy can help.
Table of Contents:
- What is urinary incontinence?
- What does the pelvic floor have to do with continence?
- Stress incontinence
- Urge incontinence
- Mixed incontinence
- What increases my risk for urinary incontinence?
- Urinary incontinence treatment
- Bottom line
What is Urinary Incontinence?
Urinary incontinence is the involuntary leakage of urine due to the loss of bladder control. It is a common condition affecting nearly 10 percent of the Canadian population.[i]
There are different types of urinary incontinence. The two most commonly assessed and treated by a pelvic floor physiotherapist are stress incontinence and urge incontinence. These two types are also the most prevalent.
What Does the Pelvic Floor Have To Do with Continence?
The pelvic floor has 5 main functions; one of which is sphincteric. The muscles of the pelvic floor control the openings of the urethra, vagina and rectum, and therefore are crucial for maintaining urinary and fecal continence.[ii]
Stress Incontinence
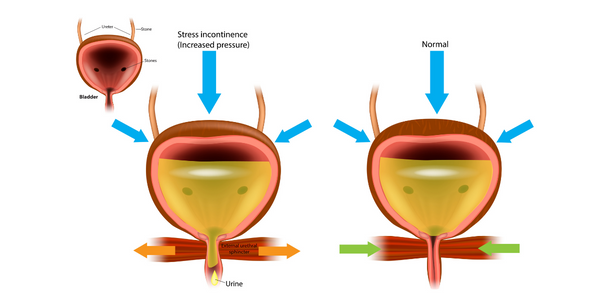
Stress incontinence is caused by an increase in intra-abdominal pressure, which increases pressure on your bladder and can lead to involuntary leakage of urine. Common activities that can cause stress incontinence include coughing, sneezing, laughing, jumping, exercising and bending.
It occurs when the pelvic floor muscles, the urethral sphincter, or both structures are weakened or dysfunctional and are unable to consistently hold in urine. The amount of leakage might range from a few drops to several tablespoons, and it can happen even when there is no urinary urge.
Urge Incontinence
Urge incontinence is a sudden, intense urge to urinate with an inability to delay voiding, followed by an involuntary loss of urine before you are able to reach the bathroom.
The walls of the bladder are mainly formed by the detrusor muscle. This muscle is responsible for contracting to push urine out of the bladder and relaxing to allow the storage of urine. Urge incontinence often occurs when the detrusor muscle becomes overactive causing it to be shortened and tight.
Mixed Incontinence
Mixed incontinence is a condition with symptoms of both stress and urge incontinence. There is leakage with increases in intra-abdominal pressure as well as an intense urge to void.
What Increases my Risk for Urinary Incontinence?
Risk factors that can increase your risk of urinary incontinence include:
- Sex: Females (individuals with internal sexual organs)
- Age (over 40)
- Obesity
- Pregnancy and Childbirth
- Obstetric trauma (forceps, suctioning, tearing)
- Gynaecological or urinary surgery
- Post menopausal
- Chronic illness
- Medication
- Smoking
- Chronic straining (ex: constipation)
- Lung conditions that result in frequent coughing
- Pelvic or prostate surgery
- Neurological conditions (Parkinson’s, Multiple Sclerosis, Spinal Cord Injury)
- Diabetes
Urinary Incontinence Treatment
Pelvic floor physiotherapy is the first-line of stress and mixed urinary incontinence treatment in people with internal sexual organs.[iii] Pelvic floor muscle training can eliminate or improve symptoms of all types of urinary incontinence. Evidence shows that it can reduce the frequency of leakage, the quantity of leakage and improve reported symptoms as well as quality of life.[iv] Pelvic floor muscle training can also be effective as a form of prevention of urinary incontinence.
Physiotherapy assessment typically involves a detailed history taking as well as an external examination. An internal examination is likely indicated to help further assess and determine the strength, tension and coordination of the pelvic floor muscles. This will help guide treatment as your therapist can provide feedback to ensure pelvic floor muscles are contracting in the correct way, as well as fully relaxing.
Depending on assessment findings, pelvic floor physiotherapy can help
- Reduce tightness or tension of the pelvic floor muscles
- Increase strength and coordination of the pelvic floor muscles
One or both of these issues may need to be addressed to manage urinary incontinence.
Treatment for urinary incontinence from a pelvic health physiotherapist may include:
- Manual techniques to facilitate pelvic floor contraction
- Manual techniques for pelvic floor relaxation
- Exercise prescription to improve mobility of affected areas
- Stress reduction to encourage relaxation of tissues
- Breathing exercises
- Guidance on progressive stretching
- Addressing/ discussing lifestyle factors such as toileting habits, constipation, hydration, nutrition, stress, relaxation, activity modification
Bottom Line
It is a misconception to think it is normal to have urinary leakage after childbirth. It is also a misconception to think it is normal to have urinary leakage as one ages. There is strong evidence to support pelvic floor muscle training as a non-invasive strategy for urinary incontinence treatment. Contact us if you want to know more about urinary incontinence and pelvic floor physiotherapy!
References
[i] FAQs | Urinary Incontinence & Stress Urinary Incontinence (SUI). (n.d.). The Canadian Continence Foundation. Retrieved October 28, 2022 from
[ii] Kegel 1947, Beji 2003, Chambless 1984, Wurn 2005, Kendall 1970, Hodes 2010, Sapsford 2009, Safik 2011.
[iii] Dumoulin C, Hay-Smith J, Berghmans B, Burgio K et al., 2016, Cochrane Collaboration.
[iv] Damoulin, Cacciari, Hay Smith, Cochrane review, September 2018. Nandy, S., & Ranganathan, S. (2022). Urge Incontinence. In StatPearls. StatPearls Publishing.
Written by