As a pelvic physiotherapist, I often work with individuals who are experiencing pain with sexual intercourse, also known as dyspareunia. Some believe it is normal. Some believe they just need to put up with it. Sexual intercourse should not be painful. Inserting a tampon, or a speculum for a vaginal exam, may be uncomfortable, but it should not be painful.
Many people do not know that they can and should seek medical care for pain with intercourse. Dyspareunia treatment from a registered physiotherapist trained in pelvic health can help resolve symptoms and lead to pain-free intercourse.
Dyspareunia is a common condition seen in the postpartum population, but can affect any individual, at any stage of their life. It is estimated that up to 58% of people experience pain with intercourse at three months postpartum. Forty percent continue to have pain at 6 months postpartum.[i]
Unfortunately, those who do seek medical care for sexual pain report believing that their concerns are invalidated and dismissed. [ii] It’s time for this to change. It’s time for healthcare professionals and the health care system to acknowledge sexual health as an element of human health and to support individuals to work towards achieving health in all domains of well-being.
In this article, you will learn more about the causes, risks factors, symptoms, and dyspareunia treatment options.
Table of Contents
- What is Dyspareunia?
- Dyspareunia Causes
- Risk Factors for Dyspareunia
- Dyspareunia Symptoms
- Dyspareunia Treatment
- Is Dyspareunia Curable?
- How Long Does It Take to Treat Dyspareunia?
- What is the Difference Between Dyspareunia and Vulvodynia?
- Bottom Line
What is Dyspareunia?
Dyspareunia is a term that indicates painful sexual intercourse in the absence of disease. Dyspareunia can also include pain with tampon insertion, speculum (i.e., PAP test), etc. It can affect any individual at any stage of life, but is more commonly reported in women versus men.[iii]
Evidence suggests that trans masculine individuals have a higher prevalence of dyspareunia than the general population.[iv] Gender confirmation surgery as well as the use of testosterone may result in tissues changes that increase the likelihood of dyspareunia. [v]
There are two main types of dyspareunia:
- Primary dyspareunia: Individual has never been able to have pain-free penetration
- Secondary dyspareunia: At some point, individual was able to have pain-free intercourse, but now it’s painful
The frequency of pain with penetration can be either constant or situational. The location of the pain can feel superficial or deep, or like a structure is getting in the way.
Unfortunately, dyspareunia can have significant consequences for an individual’s life, including physical health, mental health, body image, self-efficacy, relationships with partners, as well as efforts to conceive. [vi]
Dyspareunia can also be associated with decreased libido, decreased arousal and difficulty achieving orgasm.[vii]Seeking out a healthcare professional who you trust and takes a whole-person approach, is a great step towards management of this condition.
Dyspareunia Causes
Dyspareunia may be caused by one or a combination of the following:
Hormonal changes: Estrogen drops significantly in the postpartum period and during menopause. Low estrogen results in drying of vaginal tissues and therefore decreased tissue integrity. Vaginal atrophy is a term used to describe drying, thinning and loss of elasticity in the vaginal tissues, which may occur with menopause and contribute to dyspareunia.
Scar tissue: Scar tissue following childbirth (tear or episiotomy), surgery or trauma can result in increased sensitivity and decreased tissue mobility. This can cause pain when pressure or stretch is applied to the area.
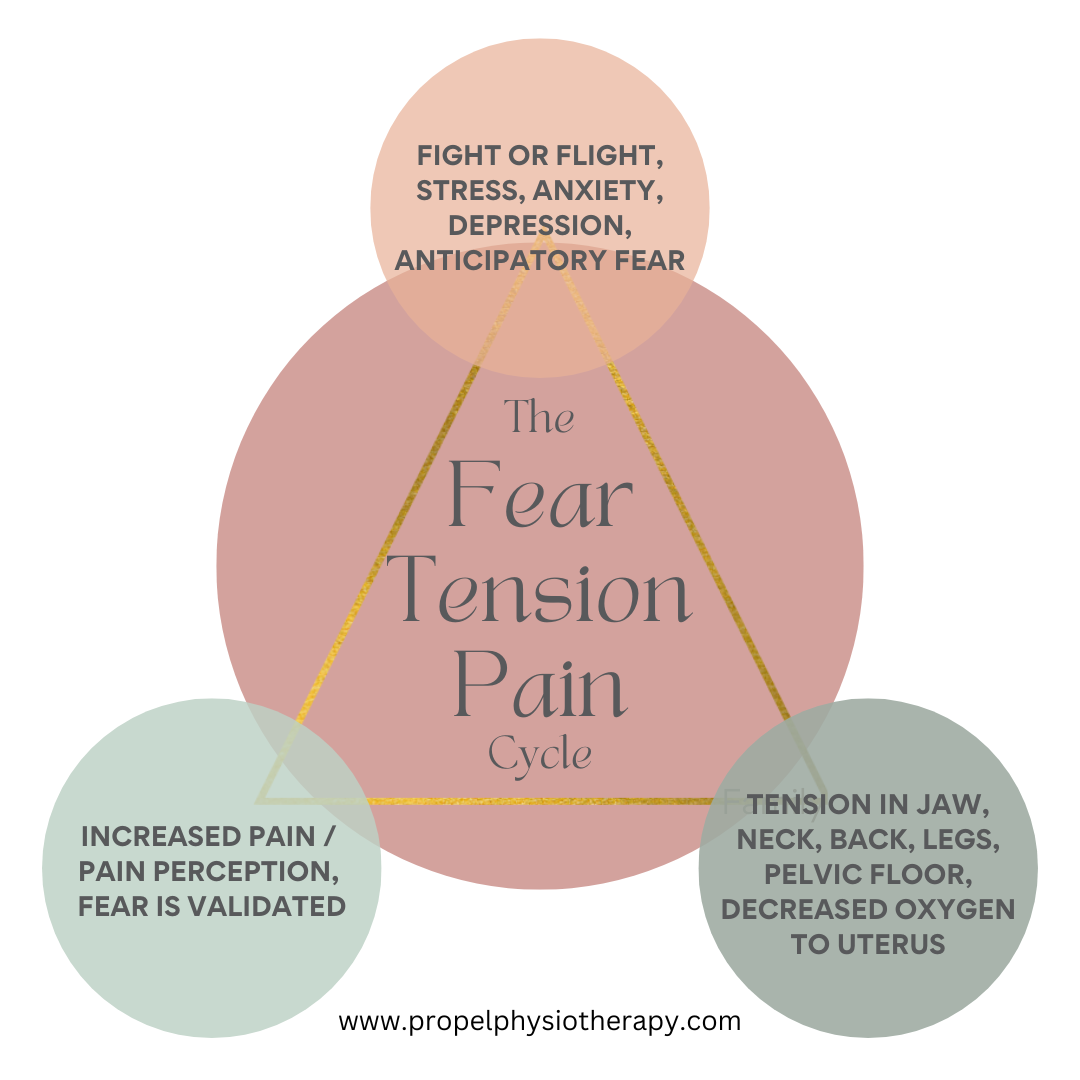
Pelvic floor muscle tension: The muscles that make up your pelvic floor play a significant role during penetration. Ideally penetration happens in a relaxed state, allowing the pelvic floor to lengthen. If these muscles are tense, tender and/or overactive, they can be a source of pain when penetration is attempted. Things that can contribute to pelvic floor tension include stress, anxiety, depression, sexual abuse, fear of physical abuse (psychological correlates)[viii]
Other pelvic conditions: Dyspareunia can be associated with other conditions such as interstitial cystitis, bladder pain syndrome, vaginismus, vulvodynia, endometriosis, pelvic inflammatory disease, polycystic ovarian syndrome and others. It can also be a protective response to infection, inflammation or injury.
Pelvic conditions that affect male reproductive organs and may contribute to dyspareunia include prostatitis, interstitial cystitis, infection of the prostate or bladder, testicular cancer, Peyronie’s disease.
Risk Factors for Dyspareunia
The following risk factors are associated with dyspareunia:
- Postmenopausal individuals
- Individuals on medication that causes vaginal dryness
- Individuals with a viral or bacterial infection
- Adolescents who experience pain with tampon insertion (4 times the risk of dyspareunia)[ix]
- Those with detrimental vulvar hygiene habits. For example, the use of vaginal cleansing products as well as vaginal douching may alter the vaginal pH and disrupt the vaginal microbiome, leading to an increased risk of tissue irritation and possibly contributing to pain with intercourse.
- Individuals who have experienced sexual abuse or have fear of physical abuse
- Individuals with anxiety
Dyspareunia Symptoms
Symptoms can vary, but include genital pain before, during or after intercourse. This could mean;
- Pain upon entry (penetration)
- Pain with every penetration (including inserting a tampon)
- Deep pain during intercourse
- Burning pain or aching pain
- Throbbing pain, lasting hours after intercourse
Dyspareunia Treatment: How a Pelvic Health Physiotherapist Can Help
Pelvic health physiotherapists are able to take a holistic approach to the assessment and treatment of dyspareunia. Assessment often includes a detailed history taking as well as an external examination of muscle tension.
An internal examination is likely indicated (but not always necessary) to help further assess and determine if tissues are protective, tender, and/or overactive. This will help guide treatment as your therapist can provide feedback and guide you to connect with areas of increased tension; allowing you to lengthen and let go of tension.
Dyspareunia treatment from a pelvic health physiotherapist may include:
- Manual techniques for internal tissue relaxation
- Exercise prescription to improve mobility of affected areas
- Stress reduction to encourage relaxation of tissues
- Breathing exercises
- Stretching of tissues or scar mobility
- Guidance on progressive stretching
- Addressing/ discussing lifestyle factors such as sleep, nutrition, hydration, relaxation, regular toileting, use of lubricant
- Education; pain science, lifestyle influence
- Guidance on use of dilators to gradually teach the muscles how to relax
Is Dyspareunia Curable?
Yes. When the appropriate support and treatment is provided, it is possible for individuals with dyspareunia to be able to have pain-free intercourse.
Treatment of dyspareunia may vary depending on the underlying cause and often a multi-disciplinary approach is recommended. Pelvic floor physiotherapy has been shown to be an effective and important aspect of treatment.[x]
How Long Does It Take to Treat Dyspareunia?
The answer to this question is variable depending on the cause and contributing factors. It is possible to see a positive change within one session with a pelvic health physiotherapist. However, full recovery (achieving pain-free penetration) often requires an individual’s full investment in the process. This means closely following the exercises and recommendations provided by the therapist for the duration of treatment plan Your practitioner will likely give you exercises, breathing strategies or relaxation techniques to work on your own.
What is the Difference Between Dyspareunia and Vulvodynia?
Vulvodynia is classified as “chronic burning, tearing, stabbing, aching vulvar pain of at least 3 months.”[xi] While dyspareunia includes pain at the vaginal entrance or deep in the pelvis, as well as pain of male reproductive organs, vulvodynia is localized to the vulva or vaginal opening. Vulvodynia is chronic in nature, whereas dyspareunia may be acute.
Pelvic health physiotherapy is an integral element of managing vulvodynia. Learn more about vulvodynia causes, symptoms and treatment.
Last Word on Dyspareunia Treatment
Similar to many pelvic health conditions, dyspareunia is common, but not normal. The Centers for Disease Control and Prevention (CDC) suggests sexual health is an intrinsic element of human health. It’s time that individuals who experience pain with intercourse have access to the support and resources to manage and treat the underlying causes.
Pelvic floor physiotherapy is an integral element of managing dyspareunia. If you have questions on how pelvic floor physiotherapy may help you, please reach out to one of our pelvic health physiotherapists.
References
[i] Lagaert L, Weyers S, Van Kerrebroeck H, Elaut E. Postpartum dyspareunia and sexual functioning: a prospective cohort study. Eur J Contracept Reprod Health Care. 2017 Jun;22(3):200-206. doi: 10.1080/13625187.2017.1315938. Epub 2017 Apr 27. PMID: 28447919.
[ii] Braksmajer A. Struggles for medical legitimacy among women experiencing sexual pain: a qualitative study. Women Health. 2018;58(4):419-433.
[iii] Tayyeb M, Gupta V. Dyspareunia. 2022 Jun 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32965830.
[iv] Abern L, Maguire K, Cook J, Carugno J. Prevalence of Vulvar Pain and Dyspareunia in Trans Masculine Individuals. LGBT Health. 2022 Apr;9(3):194-198. doi: 10.1089/lgbt.2020.0357. Epub 2022 Feb 3. PMID: 35119296.
[v] Olbedin-Maliver J. Pelvi pain and persistent menses in transgender men. June 17 2016.
[vi] Seehusen DA, Baird DC, Bode DV. Dyspareunia in women. Am Fam Physician. 2014 Oct 1;90(7):465-70. PMID: 25369624.
[vii] Tayyeb M, Gupta V. Dyspareunia. 2022 Jun 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32965830.
[viii] Landry T, Bergeron S. Biopsychosocial factors associated with dyspareunia in a community sample of adolescent girls. Arch Sex Behav. 2011 Oct;40(5):877-89. doi: 10.1007/s10508-010-9637-9. Epub 2010 Jun 22. PMID: 20567891.
[ix] ibid.
[x] Ghaderi F, Bastani P, Hajebrahimi S, Jafarabadi MA, Berghmans B. Pelvic floor rehabilitation in the treatment of women with dyspareunia: a randomized controlled clinical trial. Int Urogynecol J. 2019 Nov;30(11):1849-1855. doi: 10.1007/s00192-019-04019-3. Epub 2019 Jul
[xi] Vieira-Baptista P, Lima-Silva J, Pérez-López FR, Preti M, Bornstein J. Vulvodynia: A disease commonly hidden in plain sight. Case Rep Womens Health. 2018 Sep 12;20:e00079. doi: 10.1016/j.crwh.2018.e00079. PMID: 30245974; PMCID: PMC6142188.
Written by