Vulvodynia is a chronic pain condition that affects and estimated 8-10 percent of individuals worldwide. It is associated with many risk factors, including genetics, inflammation, and stress but vulvodynia causes vary from person to person.
Vulvodynia symptoms can have significant consequences on an individual’s qualify of life, including physical health and sexual function. The good new is that it is possible for individuals with vulvodynia to experience relief of their symptoms, and in some cases elimination of pain when the appropriate support and treatment is provided.
Pelvic health physiotherapists take a holistic approach to the assessment and treatment of vulvodynia. In this article, we take a look at closer look at how vulvodynia is diagnosed, vulvodynia causes, symptoms and risk factors.
We will also talk about vulvodynia treatment, specifically how pelvic floor physiotherapy can help, whether it is curable and just how long treatment can take.
Table of Contents
- What is vulvodynia and how is it diagnosed?
- Vulvodynia causes
- Risk factors for vulvodynia
- Vulvodynia symptoms
- Vulvodynia treatment
- Is vulvodynia curable?
- How long does it take to treat vulvodynia?
- What is the difference between dyspareunia and vulvodynia?
- Bottom Line
What is Vulvodynia and How is it Diagnosed?
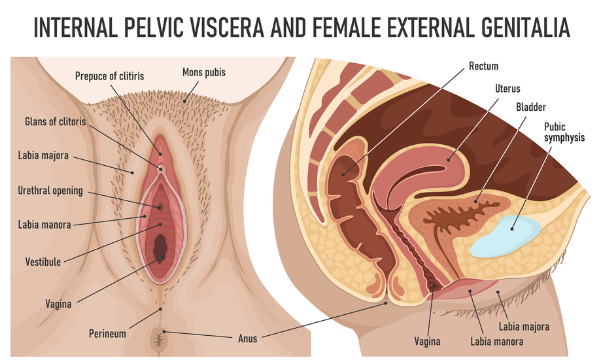
Vulvodynia is a term that describes chronic vulvar pain, without an identifiable cause. The vulva is the part of the female genitalia on the outside of the body. It includes the labia, clitoris, vaginal opening and the opening to the urethra.
Vulvodynia is most often reported as a burning pain and occurs in the absence of a specific, clinically identifiable disorder. It is therefore a diagnosis of exclusion, meaning that specific disorders such as infections, inflammatory disorders, neurologic disorders, trauma and hormonal deficiencies must be ruled out before a diagnosis is made.[i]
Vulvodynia is also a chronic syndrome meaning that painful symptoms should be present for 3-6 months before a diagnosis is considered. Unfortunately, about 40% of individuals who have this type of pain will not seek help and of those who do, 60% will see more than three health care providers.[ii]
It is estimated that worldwide, 8-10% of individuals suffer from vulvodynia at some point in their life.[iii]
Vulvodynia can be classified into two types:
1) Generalized vulvodynia
- Pain is constant
- Pain is present in throughout the entire vulva
- Typically described as “burning” pain
- Pain may be provoked, spontaneous or both
2) Localized vulvodynia
- Pain is localized to a specific part of the vulva such as the vestibule or the clitoris
- Typically described as a burning/ cutting pain at entrance of the vagina
- Pain may be unprovoked, provoked or mixed
Unfortunately, vulvodynia can have significant consequences on an individual’s quality of life, including physical health and function, mental health, body image, self-efficacy, sexual function, libido, and relationships with partners.[iv],[v],[vi]
Vulvodynia Causes
Vulvodoynia rarely has one cause and is often a result of a combination of factors. As it is a chronic pain condition, both physical and psychosocial factors play a role the development of vulvodynia. The involvement of each factor will vary from person to person.
Risk Factors for Vulvodynia
The following risk factors are associated with vulvodynia:
- Genetic predisposition: Studies suggest that some individuals with vulvodynia may have a genetic predisposition towards factors such as an exaggerated inflammatory response.
- Hormonal factors (ex: decreased estrogen): Vulvar pain is partly modulated by circulating hormones. It is therefore proposed that fluctuations in hormones may be associated with both vulvodynia and dyspareunia (pain with intercourse).
- Inflammation: It has been hypothesized that an inflammatory response to chronic infection and/or trauma to the vaginal mucosa may also increase the risk of vulvodynia.
- Pelvic floor muscle overactivity: Associations have been made between vulvodynia and pelvic floor muscle dysfunction such as hyperactivity and deficits in muscle control.
- Neurological mechanisms: Evidence suggests that there may be central mechanisms (spinal cord, brain) and peripheral mechanisms (increase in nerve fiber endings) that contribute to the development of vulvodynia.
- Psychosocial factors (ex: stress, anxiety, depression, history of abuse, family learning): Many studies have demonstrated the association between psychosocial factors and chronic pelvic pain.
- Co-morbidities: There is frequent comorbidity with other painful pelvic conditions such as painful bladder syndrome, interstitial cystitis, endometriosis and dyspareunia. Other possible comorbid conditions include fibromyalgia, irritable bowel syndrome, major depressive disorders.[vii]
Vulvodynia Symptoms
Symptoms vary, but may include one or more of the following:
- Burning
- Stabbing
- Stinging
- Itching
- Allodynia (light touch is painful such as sitting, wearing underwear)
- Hyperalgesia (a small amount of pain perceived as great)
- Functional limitations; intercourse, tampon insertion, vaginal exam, sitting, clothing
Vulvodynia symptoms may be constant, intermittent, persistent, provoked, spontaneous, mixed, immediate or delayed.
Vulvodynia Treatment: How a Pelvic Health Physiotherapist Can Help
Pelvic health physiotherapists take a holistic approach to the assessment and treatment of vulvodynia. Assessment often includes a detailed history taking as well as an external examination.
An internal examination may be indicated (but not always necessary) to help further assess and determine if tissues are protective, tender, and/or overactive. This should be completed in a gradual manor and includes continued consent and feedback from the patient. An internal assessment can help guide treatment as your therapist can provide feedback and guide you to connect with areas of increased tension; allowing you to lengthen and let go of tension.
Treatment for vulvodynia from a pelvic health physiotherapist may include:
- Education regarding vulvar care; hygiene, products (such as type of underwear, pantyliner etc), moisturizers, lubricants
- Addressing or discussing lifestyle factors such as sleep, nutrition, hydration, relaxation, regular toileting, clothing, use of lubricant
- Manual techniques for tissue relaxation
- Exercise prescription to improve mobility of affected areas
- Addressing stress, anxiety and/or depression to encourage relaxation of tissues
- Breathing exercises and guided imagery for relaxation
- Stretching of tissues or scar mobility
- Education; pain science, lifestyle influence
Treatment of vulvodynia may often require a multidisciplinary approach. If indicated, your pelvic health therapist may refer or connect you to other health care practitioners such as a psychotherapist or sexual therapist. Sometimes topical treatments provided by your doctor may be another component to address this type of pain.
Is Vulvodynia Curable?
When it comes to vulvodynia, it is important to note that not all treatments works for every individual. When the appropriate support and treatment is provided, it is possible for individuals with vulvodynia to experience relief of their symptoms, and in some cases elimination of pain.
Studies have demonstrated that pelvic floor physiotherapy along with psychological therapy can be effective treatment strategies to decrease pain and improve quality of life.[viii] This study did not show improvements in sexual function.
How Long Does it Take to Treat Vulvodynia?
The answer to this question is variable depending on the vulvodynia causes and contributing factors. It is possible to see a positive change within one session with a pelvic health physiotherapist. However, full recovery often requires an individual’s full investment in the process. This means closely following the exercises and recommendations provided by the therapist for the duration of the treatment plan.
What is the Difference Between Dyspareunia and Vulvodynia?
Dyspareunia is a term that describes pain at the vaginal entrance or deep in the pelvis, as well as pain of male reproductive organs. Dyspareunia is pain that occurs with intercourse or penetration. Vulvodynia is localized to the vulva or vaginal opening and is chronic in nature, whereas dyspareunia may be acute.
Pelvic health physiotherapy is an integral element of managing dyspareunia. Learn more about dyspareunia treatment.
Bottom Line
Vulvar pain is a prevalent condition that should not be considered as “normal”. Although vulvodynia causes are often varied and complex, symptoms can be improved with the appropriate treatment and support. Pelvic floor physiotherapy is often an integral element of managing vulvodynia. If you have questions on how pelvic floor physiotherapy may help you, please reach out to one of our pelvic health physiotherapists.
References
[i] ISSWSH, IPPS, ISSVD Consensus on vulvar pain terminology committee, 2015
[ii] Harlow B.L., Stewart E.G. A population-based assessment of chronic unexplained vulvar pain: Have we underestimated the prevalence of vulvodynia? J. Am. Med. Women’s Assoc. 2003;58:82–88.
[iii] Bergeron S., Reed B.D., Wesselmann U., Bohm-Starke N. Vulvodynia. Nature reviews. Dis. Prim. 2020;6:36
[iv] Jelovsek J.E., Walters M.D., Barber M.D. Psychosocial impact of chronic vulvovagina conditions. J. Reprod. Med. 2008;53:75–82.
[v] Arnold L.D., Bachmann G.A., Rosen R., Kelly S., Rhoads G.G. Vulvodynia: Characteristics and associations with comorbidities and quality of life. Obstet. Gynecol. 2006;107:617–624. doi: 10.1097/01.AOG.0000199951.26822.27.
[vi] Alappattu M.J., George S., Robinson M.E., Fillingim R., Moawad N., LeBrun E.W., Bishop M.D. Painful Intercourse Is Significantly Associated with Evoked Pain Perception and Cognitive Aspects of Pain in Women with Pelvic Pain. Sex. Med. 2015; 3:14–23. doi: 10.1002/sm2.52
[vii] Torres-Cueco R, Nohales-Alfonso F. Vulvodynia-It Is Time to Accept a New Understanding from a Neurobiological Perspective. Int J Environ Res Public Health. 2021 Jun 21;18(12):6639. doi: 10.3390/ijerph18126639. PMID: 34205495; PMCID: PMC8296499.
[viii] Lamvu G, Alappattu M, Witzeman K, Bishop M, Robinson M, Rapkin A. Patterns in Vulvodynia Treatments and 6-Month Outcomes for Women Enrolled in the National Vulvodynia Registry-An Exploratory Prospective Study. J Sex Med. 2018 May;15(5):705-715. doi: 10.1016/j.jsxm.2018.03.003. Epub 2018 Apr 7. PMID: 29631955; PMCID: PMC6613576.
Written by