Surgical excision is considered the gold standard of care for the treatment of endometriosis. Yet, this approach does not guarantee resolution of symptoms and reoccurrence is common.[i] Non-invasive approaches such as pelvic floor physiotherapy for endometriosis treatment can be extremely valuable to help manage symptoms such as pain, which is often a distinguishing factor of the disease.
Recently, there has been a call for better care in Canada for those experiencing endometriosis. EndoAct Canada advocates for a collaborative approach to care, recognizing the impact this disease has on both physical and mental well being.
“In their lifetime, approximately 1 in 10 girls and women, and unmeasured numbers of transgender, non-binary and gender diverse individuals, will develop endometriosis.”[ii]
Sadly, symptoms of endometriosis are often dismissed at a young age. It is estimated that there is an average 8 to 12-year delay between onset of symptoms and diagnosis of endometriosis.[iii]
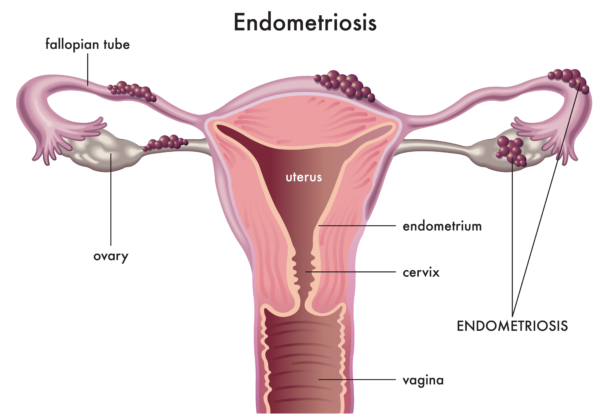
Endometriosis occurs when tissue similar to that of the lining of the uterus implants and grows outside of the uterus. The results of this can be life-altering. Endometriosis can result in significant implications on the reproductive system as well as numerous other systems of the body.
As a pelvic floor physiotherapist, I strongly believe that our profession can play a key role in providing patient-centred, individualized, holistic assessment and management strategies for those suffering from endometriosis.
In this article, I discuss the risk factors associated with endometriosis, symptoms, and both surgical and non-invasive approaches to endometriosis treatment.
Table of Contents
- What is endometriosis?
- Risk factors of endometriosis
- Symptoms of endometriosis
- Treatment of endometriosis
- How Pelvic Floor Physiotherapy for Endometriosis Helps
- Is endometriosis curable?
- Summary
What is Endometriosis?
Endometriosis refers to the growth of endometrial-like tissue on sites outside of the uterus. Growths can be found on pelvic organs (bladder, bowel, ureters, ovaries, fallopian tubes and uterus) and other pelvic structures such as ligaments, muscles and the pelvic lining. More rarely, endometriosis has been found on distant organs such as the diaphragm, lung and nasal cavity.
As the specific location of the endometriosis lesions can vary, the disease is unique from person to person. Endometriosis not only affects the reproductive system but can also affect many systems of the body including the digestive and urinary systems.
Risk Factors of Endometriosis
The exact cause of endometriosis is unknown. It is thought that there are likely multiple contributing factors including genetic, environmental and developmental.
Research is being done in this area, including the investigation of a few theories;
- Retrograde menstruation: Backward flow of menstrual tissue through fallopian tubes that deposits on pelvic organs[iv]
- Genetics/ epigenetics
- Environment exposure/ estrogen metabolism: Estrogen is a growth hormone and therefore excess estrogen may play a role in the growth of lesions
- Immune response: Immune cells may play a specific role in the invasion and growth of endometriosis cells[v]
- Circulatory or lymphatic distribution of endometriosis lesions
It should be noted that although genetics play a role in the development of endometriosis, it can affect individuals of any race from puberty to post-menopause.
Symptoms of Endometriosis
Symptoms of endometriosis may vary depending on where the growths are located, among other factors such as digestive and hormone health, diet and lifestyle. The most common symptom shared by those suffering from endometriosis is pain including.
- Chronic pelvic pain
- Dysmenorrhea (painful menstrual cycles)
- Dyspareunia (pain with intercourse)
- Back or leg pain
- Pain with exercise
- Painful bowel movements
- Bladder pain or dysfunction
Other possible symptoms of endometriosis include:
- Gastrointestinal symptoms (constipation, diarrhea, bloating, nausea and vomiting)
- Infertility
- Pregnancy loss
- Fatigue
Symptoms are often (but not always) cyclical, corresponding with an individual’s menstrual cycle.
Endometriosis Treatment
Traditionally, endometriosis has been managed by surgical intervention to remove the lesions. Surgery can be directed towards removing the lesions themselves or in some cases involves a hysterectomy. In either case, fertility can be significantly compromised.
Surgical intervention has been shown to be effective in pain relief.[vi] Unfortunately, in many cases this is short-term, with recurrence being quite common.[vii] Surgery itself also runs the risk of causing new adhesions and scar tissue formation.
For many of these reasons, non-invasive methods for treating adhesions are important. Often the best relief from symptoms is achieved when patients combine a variety of treatment strategies.[viii]
Pelvic floor physiotherapy is an example of non-invasive treatment that has evidence to support it’s role for symptom management including pain relief and functional improvement.xi
How Pelvic Floor Physiotherapy for Endometriosis Helps
Pelvic health physiotherapists have specialized training to assess and treat the pelvic area of the body (as well as the rest of the body). We have the tools to take a holistic approach to the management of endometriosis.
Assessment by a pelvic health physiotherapist includes a detailed history taking as well as an external examination of things like posture, breathing, movement patterns, muscle strength, flexibility and tension.
An internal examination is often recommended to assess the tissues of the pelvic floor including muscles, ligaments, fascia and organs.
Treatment of endometriosis by a pelvic health physiotherapist may involve;
- Manual techniques for internal tissue relaxation
- Manual techniques to address adhesions and restrictions in soft tissue mobility in both the abdomen and pelvic floor
- Exercise prescription to improve mobility of affected areas
- Stress reduction to encourage relaxation of tissues
- Addressing/ discussing lifestyle factors such as sleep, nutrition, hydration, relaxation
- Education regarding pain science, lifestyle influence
Is Endometriosis Curable?
There is no cure for endometriosis. Individuals can find complete or partial symptom relief with treatment strategies, as discussed above. Endometriosis treatment often involves a combination of medical and natural therapies and should consider both an individual’s mental and physical health.
Bottom Line
Endometriosis can be a life-altering diagnosis that may affect multiple systems of the body. Individuals who are managing endometriosis deserve a holistic, patient-centred approach that considers both mental and physical aspects of wellness.
Pelvic health physiotherapists are positioned to play a crucial role in supporting individuals through the assessment and management of this disease. With specialized training in the assessment of the pelvic area and how it relates to the rest of the body and lifestyle, pelvic health physiotherapy should be offered as a component of treatment for all individuals with endometriosis.
If you or a loved one have endometriosis or suspect you do, contact our clinic for a complimentary consultation to discuss how pelvic floor physiotherapy help you.
References
[i] Azzolino D, Spolidoro GCI, Saporiti E, Luchetti C, Agostoni C and Cesari M (2021) Musculoskeletal Changes Across the Lifespan: Nutrition and the Life-Course Approach to Prevention. Front. Med. 8:697954. doi: 10.3389/fmed.2021.697954
[i] Nirgianakis K, Ma L, McKinnon B, Mueller MD. Recurrence Patterns after Surgery in Patients with Different Endometriosis Subtypes: A Long-Term Hospital-Based Cohort Study. J Clin Med. 2020 Feb 11;9(2):496. doi: 10.3390/jcm9020496. PMID: 32054117; PMCID: PMC7073694.
[ii] 2023. The Endometriosis Network Canada. Accessed March 8, 2023.
[iii] Pugsley Z, Ballard K. Management of endometriosis in general practice: the pathway to diagnosis. Br J Gen Pract. 2007 Jun;57(539):470-6. PMID: 17550672; PMCID: PMC2078174.
[iv] Sourial S, Tempest N, Hapangama DK. Theories on the pathogenesis of endometriosis. Int J Reprod Med. 2014;2014:179515. doi: 10.1155/2014/179515. Epub 2014 Feb 12. PMID: 25763392; PMCID: PMC4334056.
[v] Abramiuk M, Grywalska E, Małkowska P, Sierawska O, Hrynkiewicz R, Niedźwiedzka-Rystwej P. The Role of the Immune System in the Development of Endometriosis. Cells. 2022 Jun 25;11(13):2028. doi: 10.3390/cells11132028. PMID: 35805112; PMCID: PMC9265783.
[vi] Chopin N, Vieira M, Borghese B, Foulot H, Dousset B, Coste J, Mignon A, Fauconnier A, Chapron C. Operative management of deeply infiltrating endometriosis: results on pelvic pain symptoms according to a surgical classification. J Minim Invasive Gynecol. 2005;12:106–112
[vii] P. Vercellini, P.G. Crosignani, A. Abbiati, E. Somigliana, P. Viganò, L. Fedele, The effect of surgery for symptomatic endometriosis: the other side of the story, Human Reproduction Update, Volume 15, Issue 2, March-April 2009, Pages 177–188, doi.org/10.1093/humupd/dmn062
[viii] Philippa Bridge-Cook, PhD. Endometriosis: a team approach to healing. Alive, January 2017. Endometriosis – alive magazine
Written by