Thumb osteoarthritis is a degenerative disease that causes wear down of the joint cartilage at the base of the thumb, resulting in pain, inflammation, and reduced mobility. Proper diagnosis and understanding of how the disease is progressing is key to determining the right approach to thumb osteoarthritis treatment and minimizing its impact.
The thumb is the most important finger of the hand, responsible for almost half of our manual function.[i] If we lose mobility, strength, or stability in the thumb joints to injury or disease, like thumb osteoarthritis, it can greatly impact our independence.
Just think about how many of us perform daily life tasks like opening a jar, turning a doorknob, using tools, or even practicing leisure activities such as crochet or painting. Without the proper use of the thumb, these tasks become very difficult, if not impossible.
In this article we will explain the main causes of thumb osteoarthritis and the symptoms that may result. In addition, we will look at treatment options and how an occupational therapist or physiotherapist can help you prevent the progression of thumb osteoarthritis.
Table of Contents:
- Anatomy of the thumb
- What is thumb osteoarthritis?
- Thumb osteoarthritis symptoms
- Diagnosing thumb osteoarthritis
- Thumb osteoarthritis treatment options
- How to minimize the effects of thumb osteoarthritis
Anatomy of the Thumb
The hand is a very complex anatomical structure responsible for full prehension and precision tasks. However, the thumb is the only finger that can oppose the other fingers and perform a prehension, a result from a long adaptation process that initiated with our ancestors.
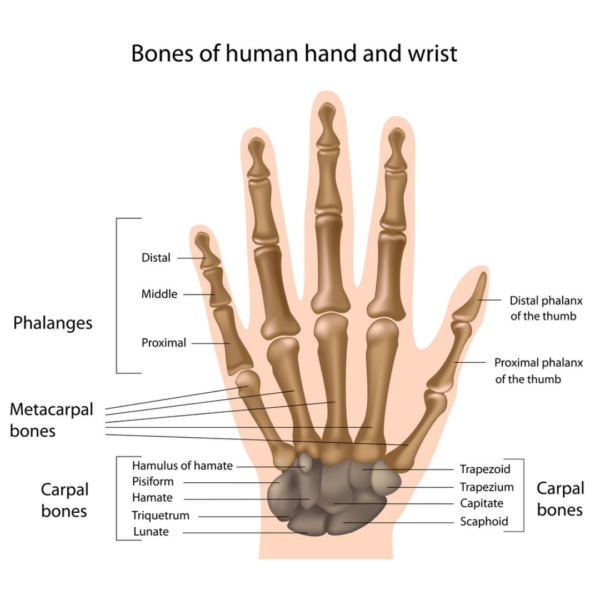
The thumb has some anatomical differences in comparison with the other fingers:
- All four fingers have three phalanges (bones that form the finger), but the thumb has only two
- The metacarpal bone (the first bone between the wrist joint and the first phalanx) is shorter
Therefore, the thumb is a shorter finger. However, is the only one that has a joint that connects the metacarpal bone and the carpus bone (trapezium), at the wrist area, in a shape of a “saddle joint.” This joint allows the thumb to rotate and in conjunction with the ligaments and muscles contributes to the stability and dexterity of any grasp.[i]
Biomechanically the joint at the base of the thumb, the carpometacarpal (CMC), endures forces 10 times more than the other joints in the hand since the thumb is involved in all forms of grasp. Overtime, with overuse and aging it is very common to develop what is called thumb osteoarthritis.
What is Thumb Osteoarthritis?
Any osteoarthritis (OA) is caused by a wear down of the joint’s cartilage. OA, also known as “wear-and-tear” arthritis, is a degenerative arthritis that progresses as you age.
With overuse of the thumb, the cartilage at the joint wears away and no longer protects the bones from rubbing against each other when moving the thumb. This causes an inflammatory and degenerative process.
Thumb osteoarthritis occurs commonly with aging. It is 10 to 20 times more predominant in women after 50 years old of age, affecting the saddle joint of the thumb.
Thumb Osteoarthritis Symptoms
Thumb osteoarthritis symptoms can include the following:
- Pain at the base of the thumb
- Swelling
- Decreased strength when trying to use the thumb
- Deformity at the joint
The use of the thumb becomes more painful as the degeneration progresses and we naturally start protecting the thumb from moving. By trying not to use the thumb, the muscle strength decreases, and other issues may occur as we are not using the hand appropriately.
Swelling of the joint and reduced mobility interfere with the ligaments. The ligaments start to wear down as the joint loosens. As a result, there is less stability at the joint to perform some of the daily tasks. With less stability the pain increases and some deformity of the joint can be formed.
Diagnosing Thumb Osteoarthritis
An examination by your doctor is necessary to diagnose thumb osteoarthritis. X-ray images will also help to identify at which level the joint has been damaged. This will help determine the best treatment approach — surgical or a more conservative non-surgical approach.
Thumb Osteoarthritis Treatment Options
At any stage of thumb osteoarthritis, it is important to learn how to manage the symptoms and protect the joint at the base of the thumb.
Non-surgical management techniques include recommendations:
- From your doctor:
- Use of anti-inflammatory medication and steroid injections to address pain and inflammation.
- From your physiotherapist or occupational therapist:
- Use of anti-inflammatory treatment techniques to reduce manage pain and swelling.
- Prescribed exercises to maintain grip strength when the pain is reduced.
- Education regarding “joint protection” adaptations while performing daily tasks.
- From a hand therapist:
- A prescription and/or fabrication of a splint for joint support.
In advance stages and when the conservative treatment no longer provides any benefit, your doctor may suggest a surgical intervention. The surgical treatment option can be discussed with your doctor as there are few techniques that they may choose from depending on your specific case.
How to Minimize the Effects of Thumb Osteoarthritis
The following steps can help you to minimize the effects of thumb osteoarthritis so you can continue to live your life to the fullest:
- Get a proper diagnosis and understand which stage you are in regarding the joint integrity of the thumb. This is fundamental to determine what treatment you require.
- Understand the injury and learn how to best use your hands avoiding the activities that may aggravate the symptoms. For example, extreme sports that required a lot of us of grip strength (i.e., rock climbing), activities that require repetitive movements like knitting and sewing.
- Use adaptive equipment such as jar opener, adapted scissors, a larger pen may help in maintaining your ability to continue using your hand without causing more stress at the thumb.
Talk to your physiotherapist or occupational therapist who will be able to make the specific recommendations for you to continue to be independent in performing the activities that you need and enjoy in your daily life.
References
[i] Ingram, J.N., Kording, K.P., Howard, I. S., and Wolpert, D.M. (2008). The statistics of natural hand movements. Exp. Brain Res. 188, 223-236.
[ii] Neumann, D.A., and Bielefeld, T. (2003). The carpometacarpal joint of the thumn: stability, deformity, and therapeutic intervention. J.Orthop, Sports Phys. Ther. 33, 386-399.
Arthritis of the Hand and Upper Extremity: A Master Skills Publication, SZ Glickel, RA Bernstein (Eds.), American Society for Surgery of the Hand, Rosemont, IL (2011), 442 pages. (2012): 1508-1509.
Heineman, John T., et al. “A Randomized Controlled Trial of Topical Cannabidiol for the Treatment of Thumb Basal Joint Arthritis.” The Journal of Hand Surgery(2022).
Spaans, Anne J., et al. “Conservative treatment of thumb base osteoarthritis: a systematic review.” The Journal of hand surgery1 (2015): 16-21.
Written by