Spine osteoarthritis is a complex degenerative disease that can cause pain and stiffness and make it more difficult to do the things you love. Despite what the medical community thought for years, it is not caused by wear and tear and also may not cause any pain. This is good news for those who want to continue to enjoy being active.
In this blog we will discuss what spine OA is, what causes it, the symptoms, and how exercise guided by a registered physiotherapist can help manage this condition.
Table of Contents
- What is spine OA?
- Causes of spine OA
- Common symptoms of spine OA
- How can exercise help spine OA
- Treatment and exercise options for spine OA
- How your physiotherapist can help
What is Spine OA?
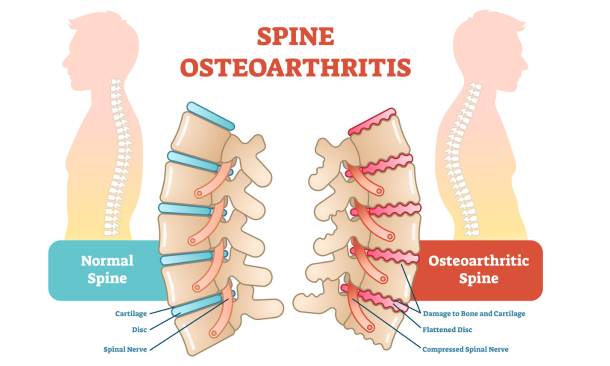
Spine OA is also known as degenerative disc disease (DDD), considered a complex multifactorial disease. It affects the joints of the spine, either the disc between the vertebrae or the facet joints which are bones that help connect vertebrae together.
Spine osteoarthritis (OA) is much more common than most realize. An estimated 40 percent of adults over the age of 40 show OA in the lumbar spine on X-ray.
The discs in the spine help protect the vertebrae and also aid in allowing the spine to absorb forces. With spine OA, as the disc degenerates in spine OA there can be pain, swelling, and stiffness at the affected joints.
Scientists used to think that spine OA was due to ‘wear and tear’. They also believed the severity of the degeneration had a direct correlation with the amount of pain you would experience. We now know that not everyone who has spine OA on imaging has symptoms.
Causes of Spine OA
OA, often referred to just as arthritis, is much more complex than previously thought. Spine OA as with other forms of OA has many factors including an inflammatory process, metabolic factors, cartilage and/or bone breakdown.
It is not necessarily clear what the exact cause is for one individual may be due to the many factors that can contribute to the disease. The current consensus is that although there are many factors, OA does involve a specific inflammatory process which causes the degeneration, not ‘wear and tear’.
Some of the most well-known risk factors include:
- gender (with women being affected more than men),
- age,
- and weight.
Common Symptoms of Spine OA
Symptoms of spine OA will vary from person to person. The most common symptoms are:
Pain: Most commonly in the lower back or neck where the most common sites of spine OA are
Decreased Range of Movement: Less mobility of the spinal joints making bending and twisting more difficult
Stiffness: Often feeling increased stiffness in the morning more than evening, tends to ease with movement
How Exercise Can Help Spine OA
Exercise is considered one of the most beneficial interventions for spine OA. Introducing or continuing to exercise can aid in increasing bone mineral density, improving mobility, and reducing pain.
One of the most important things to remember when exercising and living with spine OA is that hurt does not equal harm. Mild amounts of pain are okay to exercise with and can lead to an overall pain reduction and function increase in the long term. The spine is a very robust system and like all of the bones and joints in the body, requires exercise and movement to stay strong and prevent further decline.
Treatment and Exercise Options for Spine OA
Although there are invasive options such as spinal fusion, surgery has not been shown to be more effective than conservative management for spine OA. These non-invasive options include:
Education: understanding osteoarthritis and the spine can help manage and avoid flare ups. Understanding the condition can lead to increasing activities through lifestyle modification such as pacing.
Core Strengthening: can be very light or more intense work which helps your spine stay strong, flexible, and functional. Examples include bridges, bird-dog, dead bug, and a squat or sit-to-stand.
General Strengthening: helps manage symptoms as well as maintain or improve strength and function of your joints and muscles. Examples include walking, biking, swimming, and yoga
Aquatic Therapy: Due to the low impact and buoyancy effect in water, aquatic therapy can be a great way to increase exercise in Spine OA and increase time exercising pain free. Aqua therapy can include strength, range of motion, and endurance with much less impact on the spine. Examples include water walking, water marching, water leg lifts and core exercises while floating with a pool noodle
Pain Management: Physical Therapists typically recommend heat or cold therapy and can provide manual therapy to help relieve pain.
How Your Physiotherapist Can Help
Although hurt does not equal harm and the spine is very robust, your physiotherapist can help guide you through the process of getting stronger and reducing your pain while tailoring a program specific for you. Some people with spine OA can do Olympic lifts and pick up 200lbs from the ground, while others may require lighter exercise, biking, or water/aqua therapy.
Because levels of pain, disease progression, and function can vary widely from person to person, having a conversation with your physiotherapist on where to get started is typically the best course of action. This will help to prevent any further injuries, especially for those that that do need to be more cautious.
References
Goode, Adam P., et al. “Low Back Pain and Lumbar Spine Osteoarthritis: How Are They Related?” Current Rheumatology Reports, vol. 15, no. 2, 11 Jan. 2013, https://doi.org/10.1007/s11926-012-0305-z.
Jarraya, Mohamed, et al. “A Longitudinal Study of Disc Height Narrowing and Facet Joint Osteoarthritis at the Thoracic and Lumbar Spine, Evaluated by Computed Tomography: The Framingham Study.” The Spine Journal: Official Journal of the North American Spine Society, vol. 18, no. 11, 1 Nov. 2018, pp. 2065–2073, pubmed.ncbi.nlm.nih.gov/29679729/, https://doi.org/10.1016/j.spinee.2018.04.010. Accessed 16 Apr. 2022.
Lindsey, Thomas, and Alexander M. Dydyk. “Spinal Osteoarthritis.” PubMed, StatPearls Publishing, 2020, www.ncbi.nlm.nih.gov/books/NBK553190/.
Saltychev M, Eskola M, Laimi K. Lumbar fusion compared with conservative treatment in patients with chronic low back pain: a meta-analysis. Int J Rehabil Res. 2014 Mar;37(1):2-8. doi: 10.1097/MRR.0b013e328363ba4b. PMID: 23820296.
Written by