Physiotherapy is an important component in the management of temporomandibular joint (TMJ) disorders, which are commonly associated with pain, restricted jaw mobility, and impaired functional activities such as chewing and speaking. Dysfunction of the TMJ often arises from muscular imbalances, joint restrictions or hypermobility, postural abnormalities, and habits such as clenching or grinding teeth.
Physiotherapists employ evidence-based interventions—including manual therapy, therapeutic exercise, neuromuscular re-education, and postural retraining—to alleviate pain, restore joint mobility, and optimize functional movement patterns.
In this blog we look at the anatomy of the TMJ, symptoms of TMJ disorders, and how physiotherapy can help with the management of TMJ dysfunction.
Table of Contents:
- Anatomy of the TMJ
- Common symptoms of TMJ disorders
- Role of physiotherapy in TMJ disorder management
- Clinical practice
- Conclusion
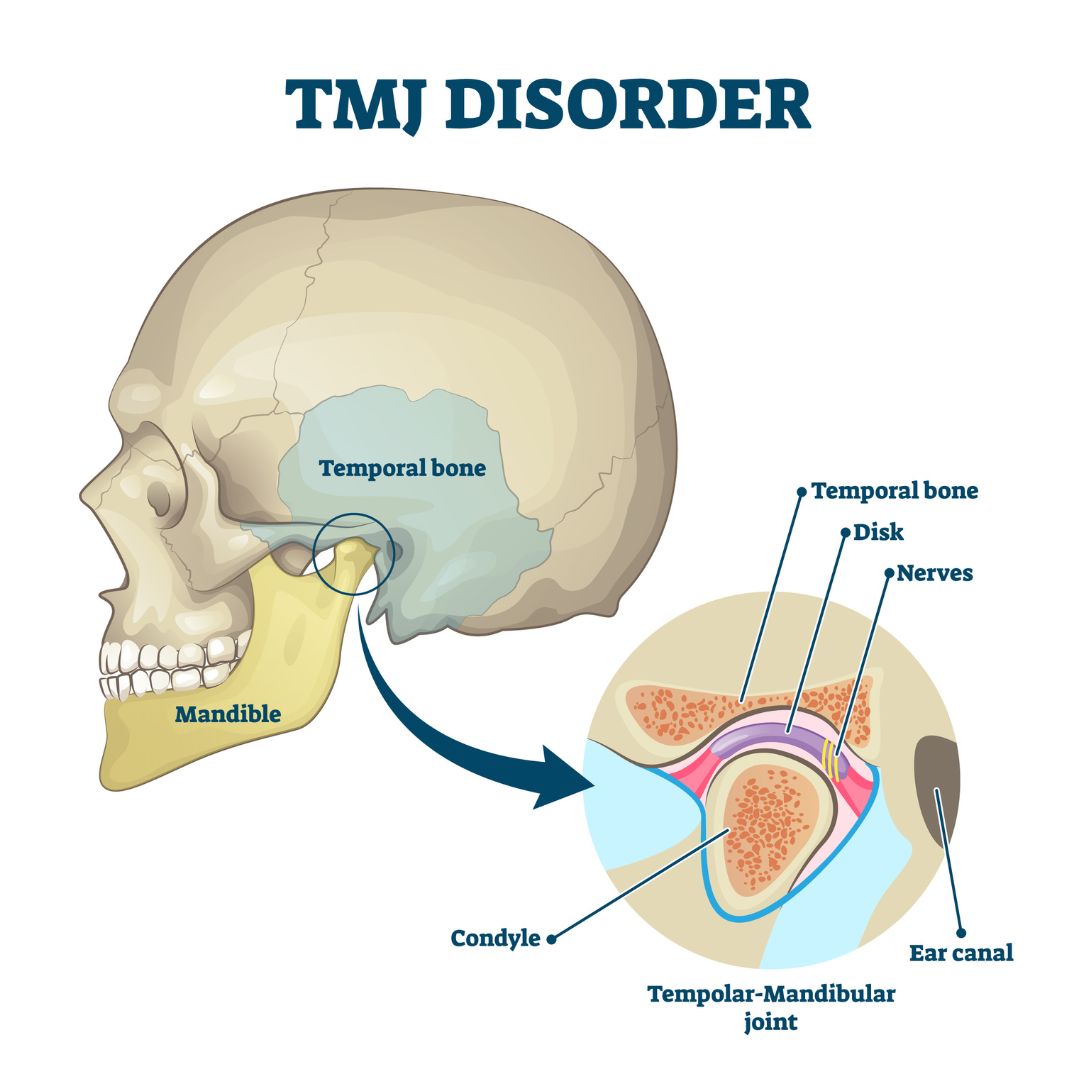
Anatomy of the TMJ
Think of your jaw joint (the Temporomandibular Joint or TMJ) as a well-engineered hinge and slide system that lets you talk, chew, and yawn.
Its anatomy includes the following key structures:
The Bony Parts: The Ball and Socket
- The “ball” is the rounded end of your jawbone (the condyle).
- The “socket” is a shallow groove in your skull that the ball fits into.
- Key Fact: These bone ends are covered with a tough, durable cartilage (like a strong eraser) built to handle a lifetime of chewing.
The Shock Absorber: The Disc
- Between the ball and socket is a small, cushiony disc.
- This disc acts like a shock absorber, keeping the bones from grinding against each other.
- It divides the joint into two sections, which allows for two different types of movement (see below).
The Support System: Ligaments and Capsule
- A strong, fibrous capsule surrounds the entire joint like a sleeve.
- Ligaments act like tough, flexible ropes that connect the bones and hold everything in place, preventing the jaw from dislocating.
The Motors: The Muscles
- The power for your jaw comes from your chewing muscles (the main ones are the Masseter and Temporalis, which you can feel on the side of your face and head).
- These muscles control all jaw movements: closing for biting, opening for yawning, and shifting side-to-side for grinding food.
The Movements: Hinge and Slide
- This is the cool part! Your jaw joint has two settings:
- The Hinge: When you first open your mouth a little (like to say “ah”), the lower part of the joint acts like a simple hinge, just rotating open.
- The Slide: When you open wide (like for a big bite), the entire “ball” (and the disc) slides forward out of the socket and down the slope of the bone. This combination of hinge and slide is what gives your jaw its wide range of motion.
Your jaw joint is a hinge that can also slide. It’s built with a tough, shock-absorbing disc to protect the bones and is controlled by powerful chewing muscles, all held securely in place by strong ligaments.
Common Symptoms of TMJ Disorders
Temporomandibular joint (TMJ) disorders can have a wide range of symptoms, often affecting not just the jaw but also the face, head, and neck. Evidence has shown a relationship between TMJ dysfunction and head and neck posture.[i]
Common symptoms include:
- Jaw pain or tenderness – usually felt in front of the ear, on one or both sides.
- Clicking, popping, or grating sounds when opening or closing the mouth.
- Difficulty or discomfort with chewing – sometimes the jaw feels like it “catches” or locks.
- Limited mouth opening or stiffness in the jaw.
- Headaches – especially tension-type headaches or pain radiating to the temples.
- Ear-related symptoms – such as earache, ringing in the ears (tinnitus), or a feeling of fullness (without infection).
- Facial pain – aching or tightness in the cheeks, temples, or jaw muscles.
- Jaw deviation – the jaw shifts to one side when opening or closing.
- Neck and shoulder pain – due to muscle tension and poor posture.
TMJ symptoms often worsen with stress, teeth clenching, grinding (bruxism), chewing hard foods, or poor posture.
Role of Physiotherapy in TMJ Disorder Management
Physiotherapy plays an important role in the management of TMJ disorders by addressing both pain and functional limitations. TMJ problems often cause jaw pain, stiffness, clicking, headaches, and difficulty with chewing or speaking. Physiotherapy aims to restore normal joint mechanics, reduce muscle tension, and improve overall jaw function.
Here are the key roles of physiotherapy in TMJ management:
- Pain relief – Techniques such as manual therapy, soft tissue release, ultrasound, TENS, and heat/cold applications help reduce joint and muscle pain.
- Improving joint mobility – Mobilization of the TMJ and surrounding soft tissues helps restore smooth movement and reduce stiffness.
- Muscle relaxation and strengthening – Exercises target overactive jaw muscles (like the masseter) while strengthening weaker muscles for better balance and stability.
- Postural correction – Since poor posture (especially forward head position) can aggravate TMJ dysfunction, physiotherapy includes neck and upper back exercises to improve alignment.
- Education and self-management – Patients learn about proper jaw use, relaxation strategies, and avoiding habits such as clenching, nail biting, or chewing gum.
- Functional training – Gradual retraining of chewing, speaking, and yawning movements ensures more efficient and less painful use of the jaw.
Systematic reviews have found that manual therapy and exercise have been found to reduce pain and improve joint mobility in TMJ disorders.[ii] By combining manual therapy, exercise, and education, physiotherapy not only relieves TMJ pain but also helps prevent recurrence and improves quality of life.
Clinical Practice
Clinically, I often see patients with TMJ issues after any injuries or surgeries to the head. This can occur from whiplash and neck injuries after motor vehicle collisions which can affect the muscles and joints in the neck causing pain in the jaw and face. Injury to the upper cervical spine and muscles in the neck can have an effect on the mechanics of the TMJ leading to pain and discomfort.
The temporomandibular joint can also be affected after a craniotomy or craniectomy, a surgery after a brain injury, stroke or brain tumour that affects the muscles of the head and face. The surgery can cut through the muscles surrounding the TMJ and thereby effect the movement and function of this joint.
Scar massage, mobility exercises, manual therapy and acupuncture can be effective at alleviating pain in this area. It is important to consider the assessment and treatment of the TMJ as it is often overlooked when treating complex and multi- injury clients.
Conclusion
Physiotherapy plays a vital role in the conservative management of temporomandibular joint (TMJ) disorders by addressing both pain and functional impairments. Through a combination of manual therapy, therapeutic exercises, postural retraining, and patient education, physiotherapists help restore optimal joint mechanics, reduce muscular tension, and improve jaw mobility.
Importantly, physiotherapy also emphasizes long-term self-management strategies that empower individuals to modify contributing factors such as poor posture, stress, and habits such as clenching or grinding the teeth.
By targeting the underlying biomechanical and musculoskeletal contributors to dysfunction, physiotherapy not only alleviates symptoms but also enhances overall quality of life and reduces the risk of recurrence in patients with TMJ disorders.
References
[i] J. Appl. Oral Sci. 17 (3) • June 2009, The relationship between temporomandibular dysfunction and head and cervical posture. https://doi.org/10.1590/S1678-77572009000300014
[ii] González-Sánchez B, García Monterey P, Ramírez-Durán MDV, Garrido-Ardila EM, Rodríguez-Mansilla J, Jiménez-Palomares M. Temporomandibular Joint Dysfunctions: A Systematic Review of Treatment Approaches. J Clin Med. 2023 Jun 20;12(12):4156. doi: 10.3390/jcm12124156. PMID: 37373852; PMCID: PMC10299279.
Written by