Duchenne muscular dystrophy (DMD) is one of the most common forms of muscular dystrophy. Muscular dystrophy is a group of more than 30 inherited muscle diseases that cause progressive weakness in the muscles that control movement.
Symptoms vary based on the type of muscular dystrophy, the muscles involved, how fast the disease progresses, and the age when diagnosed. In this article, we will look at the cause, signs and symptoms, as well as potential Duchenne muscular dystrophy treatment strategies.[i]
Table of Contents
- What is Duchenne Muscular Dystrophy (DMD)?
- What Causes Duchenne Muscular Dystrophy?
- Duchenne Muscular Dystrophy Symptoms
- Early Sings of Duchenne Muscular Dystrophy
- Diagnosing Duchenne Muscular Dystrophy
- Disease Progression and Outlook
- Duchenne Muscular Dystrophy Treatment Strategies
What is Duchenne Muscular Dystrophy (DMD)?
Duchenne muscular dystrophy is a genetic disorder that causes muscles to get progressively weaker as you age. Individuals with DMD are unable to produce the muscle protein called dystrophin that helps keep muscle cells intact. Signs of weakness typically begin between ages 3 and 5 (sometimes earlier), and the weakness typically starts in the hips and legs.
Duchenne muscular dystrophy has the most severe clinical presentation out of all forms of muscular dystrophy. In Europe and North America, DMD occurs in 6 out of every 100 000 individuals,[ii] primarily affecting boys.
What Causes Duchenne Muscular Dystrophy?
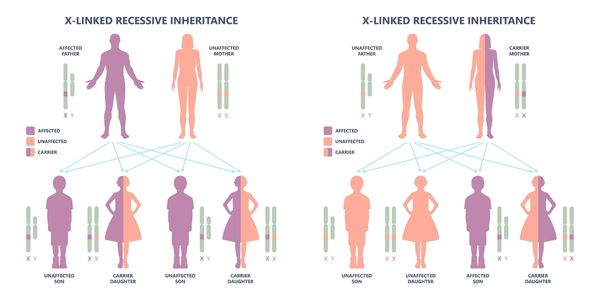
Duchenne muscular dystrophy is an X-linked recessive disorder. There is a gene in the body that is responsible for creating dystrophin, which is a muscle protein that keeps muscles strong and healthy. DMD is caused by a mutation in the dystrophin gene, which causes dystrophin to be made improperly. This causes the muscle cells to become weak and eventually break down.
Approximately one third of the time, DMD is caused by a new mutation in the gene. The other two thirds of the time, the mutated gene is inherited by the son from a mother who is a carrier of the faulty gene.[iii]
Chromosomes are the structures in our bodies that contain genetic material. Girls inherit two X chromosomes, one from their mother and one from their father. Boys inherit an X and Y chromosome, an X chromosome from their mother, and a Y chromosome from their father.
The dystrophin gene is carried on the X chromosome, so if a mother passes on an X chromosome which has a mutated copy of the dystrophin gene, her son will develop DMD. Girls who inherit a mutated copy of the gene also inherit a normal copy of the dystrophin gene on the X chromosome from their fathers. They will not develop DMD, although they will be carriers of the condition and can pass on DMD to their sons in the future.iii
DMD Carriers: A woman who is a carrier of the DMD gene has one altered X chromosome, and one normal X chromosome. Some women who are carriers experience increasing muscle weakness and fatigue, known as carrier symptoms. Since the heart muscle can be affected, women who are carriers of the DMD gene should have their heart checked regularly.iii
Duchenne Muscular Dystrophy Symptoms
- Frequent falls
- Difficulty running as quickly as their peers
- Difficulty climbing stairs
- Difficulty getting up from a chair
- Overdeveloped calf muscles
- Frequently walk on their toes and lean backwards to maintain their balance
- Progressive weakness will eventually make walking more difficult, and they will need to start using a wheelchair. All muscles will eventually become weak, including the muscles that control breathing and the heart.
- Children with DMD may develop scoliosis and muscle contractures as they growiii
Early Signs of Duchenne Muscular Dystrophy
- List
Diagnosing Duchenne Muscular Dystrophy
Duchenne muscular dystrophy is diagnosed through a combination of physical examination by a physician which will reveal weakness particularly in the proximal muscles of the body, overdeveloped calf muscles, and the following:
- Blood test showing elevated CK (creatine kinase) levels in the blood indicating there is muscle damage
- DNA blood testing (genetic testing) showing a change in the dystrophin gene
- If the DNA testing is normal, a muscle biopsy can be done which will show a lack of dystrophin in the muscle cellsiii
Disease Progression and Outlook
Muscle weakness from Duchenne muscular dystrophy can start as early as age 2 to 3 years old and affects the muscles closest to the trunk (hip and shoulder muscles) first. The muscles of the lower extremities tend to be affected before the upper extremities.ii
Over time, the muscle weakness spreads from the larger muscles close to the trunk to the muscles in the extremities. At first, children will still be able to walk, although they will adopt a toe-walking gait with an increased lumbar lordosis (inward curve in the lower part of their spine) to keep their balance.
This walking pattern causes them to develop large calf muscles to compensate for the weakness in their hip muscles. They will have difficulty with movements that require power from the hip muscles such as ascending stairs and getting up from the floor or from a chair.iii
Eventually, the muscles of the heart and the breathing muscles are also affected. Scoliosis (curvature of the spine) often develops and along with respiratory muscle weakness can impair pulmonary function and eventually cause acute respiratory failure.ii
Duchenne muscular dystrophy is a fatal condition. Boys with this diagnosis previously died in their teenage years; however, with advances in cardiac and respiratory care, many are living into their twenties and even thirties.ii
Duchenne Muscular Dystrophy Treatment Strategies
Although there is currently no cure for Duchenne muscular dystrophy, research is being done on therapies to target and replace the mutated gene to allow for the production of the missing protein dystrophin.iii
Current Duchenne muscular dystrophy treatment strategies can include physiotherapy, medication, specialized equipment prescription and surgery.
Duchenne Muscular Dystrophy Physiotherapy:
- Exercises to maintain muscle strength and function for as long as possible
- Stretching to maintain range of motion in the joints
- Referrals and recommendations for splinting to support the alignment of the ankle
- Activity modification and recommendations for physical activity and adaptive sports including: swimming, cycling, adaptive skiing, sledge hockey, wheelchair basketball, etc.
- Recommendations and training on the use of gait aids and accessible equipment for the homeiii
Medications:
- Deflazacort – a steroid medication that can help to preserve muscle strength for some time but has significant side effects. Boys who take Deflazacort are typically able to continue walking for much longer than boys who don’t, sometimes to the age of 12 or older. Boys generally start taking steroid medication around 6-8 years old when they show signs of muscle weakness such as toe walking, increasing falls, and difficulty climbing stairs.iii
- Alendronate – loss of calcium in the bones is a side effect of steroid use and immobility. This medication is used in DMD to preserve calcium levels in the bone to help prevent fractures.
Other Duchenne Muscular Dystrophy Treatments:
- Neurologists monitor the condition and disease progression of individuals with DMD, prescribe medications, and can refer to other specialists.iii
- Certified orthotists can fabricate and fit braces to improve function and manage contractures
- Occupational therapists can prescribe equipment for the household and school to allow children with DMD to function better in their environment
- Orthopaedic surgeons can treat severe scoliosis or contractures that cannot be managed with bracing
- Cardiologists monitor heart function
Congenital Muscular Dystrophy
In addition to Duchenne Muscular Dystrophy, there are at least 33 other types of congenital muscular dystrophies with varying presentations. Congenital muscular dystrophies are a group of conditions with muscle weakness that start in infancy or early childhood (typically before the age of 2).
Boys and girls can both be affected by congenital muscular dystrophy. The presentation and progression of the condition, as well as the treatment will depend on the type of congenital muscular dystrophy an individual has.iii
Physiotherapists are an important part of the clinical management team for individuals with muscular dystrophy and the clinicians at Propel Physiotherapy have extensive experience treating clients with neurological conditions. If you have any questions about physiotherapy treatment for muscular dystrophy, or would like to book a complimentary consultation with one of our clinicians at Propel Physiotherapy, please reach out to us at info@propelphysiotherapy.com, or 866-210-6303.
References
[i] https://www.hopkinsmedicine.org/health/conditions-and-diseases/duchenne-muscular-dystrophy#:~:text=DMD%20is%20a%20genetic%20disease,muscles%20require%20to%20function%20normally
[ii] https://www.mda.org/disease/duchenne-muscular-dystrophy
[iii] https://muscle.ca/wp-content/uploads/2019/09/DuchenneMuscularDystrophy-E.pdf
Written by