Spinal muscular atrophy or SMA is a genetic muscle-wasting disorder that affects 1 in 6,000 to 1 in 10,000 births. SMA can delay development, make chewing and swallowing difficult and in some cases can be fatal. Although, there is no cure for SMA, there are various forms of spinal muscular atrophy treatment.
There are four types of SMA that vary in severity, prognosis and symptoms onset. Spinal muscular atrophy treatment depends on the type and severity of symptoms. In general, cases include varying degrees of muscle weakness, fatigue, and respiratory issues among other symptoms.
In this article we will look at the causes, diagnosis, types of SMA, as well as potential spinal muscular atrophy treatments.
Table Contents
- What is Spinal Muscular Atrophy?
- What Causes Spinal Muscular Atrophy?
- How is Spinal Muscular Atrophy Diagnosed?
- Possible Signs and Symptoms of Spinal Muscular Atrophy
- Types of Spinal Muscular Atrophy
- Physiotherapy for Spinal Muscular Atrophy
- Other Spinal Muscular Atrophy Treatment
What Is Spinal Muscular Atrophy?
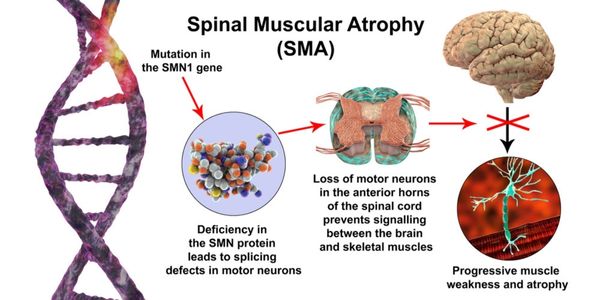
Spinal muscular atrophy (SMA) is a group of genetic muscle-wasting disorders that affect the nerve cells supplying muscles. These conditions cause the nerve cells (motor neurons) to die off, which impairs the signal travelling to the muscles. When this signal is disrupted, the muscle is unable to function like normal and it becomes weak.
The large muscles closer to the body are more disrupted than the smaller muscles further away in the extremities. In some cases, facial muscles are affected; and in severe cases, the muscles used for breathing and swallowing can become weak.
Spinal muscular atrophy (SMA) can affect males or females, and the age of onset is determined by the SMA subtype.[i]
What Causes Spinal Muscular Atrophy?
SMA is an autosomal recessive condition, in other words, passed down through a mutated gene from both parents to the child. It is often seen in families who have no previous history of the condition. This condition has an incidence of 1 in 6000 to 1 in 10 000 births.[ii]
The majority of cases of spinal muscular atrophy are caused by a deletion or mutation of the Survival Motor Neuron (SMN) gene, located on chromosome 5. There are two different types of the survival motor neuron gene, SMN 1 and SMN 2. The deletion of the SMN 1 gene is what causes the disorder, while the severity of the disorder is determined by the number of copies of the SMN 2 gene present.[i]
How Is Spinal Muscular Atrophy Diagnosed?
Individuals are typically diagnosed with SMA by a physician using a combination of medical history, physical examination, and diagnostic testing. In the early stages of SMA type I, the diagnosis may be suspected due to an infant’s floppiness and lack of head control, with minimal to absent anti-gravity movements and respiratory complications.[iii]
Diagnostic testing for SMA includes:
- Clinical examination and labs – blood tests determine the amount of creatine kinase present – elevated levels can indicate that muscle damage has occurred[iii]
- Muscle biopsy – a small portion of muscle tissue is removed and examined surgically under a microscope for changes that are characteristic of SMA.[i]
- Electromyogram (EMG) – needles are placed into portions of the muscle. Specific types of electrical activity in the muscle can be indicative of SMA.[i]
- Genetic testing – can be used prenatally in couples who have a child with SMA and who are pregnant with another child. In many cases, genetic testing can also be used in place of a muscle biopsy for diagnosis of SMA in infants and children. This is the most accurate type of testing for diagnosing Spinal Muscular Atrophy.[i]
Possible Signs and Symptoms of Spinal Muscular Atrophy
Symptoms of SMA can vary depending on the type of spinal muscular atrophy (see descriptions below) but can include:
- Muscle weakness, with proximal muscles (closer to the body) being more affected than distal muscles
- Fatigue
- Loss of reflexes
- Scoliosis (curvature of the spine) – as growth and alignment of the spine relies partially on normal muscle activity
- Respiratory issues
- Swallowing difficulties and choking episodes[i]
SMA Types
There are four primary types of SMA:
SMA Type I
Also known as infantile progressive spinal muscular atrophy, this type of SMA usually appears within the first 6 months of life. These infants will exhibit poor cough and feeding, increased breathing rate, and inability to sit independently.
Chest infections are common in this group due to the weakness of their chest and breathing muscles, and inability to clear secretions effectively. This type of SMA is usually fatal within the first two years and is the most common genetic cause of infant mortality.[i]
Symptoms:
- Neonatal hypotonia (low muscle tone)
- Severe generalized muscle weakness, with some infants being almost completely immobile
- Weakened muscles affecting crying, sucking, breathing, and swallowing
- Frequent chest infections
- Survival beyond the third year of life is rare.
SMA Type II
Also known as intermediate SMA, it is typically diagnosed within the first year to eighteen months of life. This form is not as severe as SMA type I, but the symptoms are similar. It may be impossible to distinguish between the two in the first year.
These infants are often able to sit independently, but unable to stand or walk independently. The spine and respiratory muscles can be involved in this type of SMA. The outcomes for children with SMA type II depends on the degree of respiratory involvement.[i]
Symptoms:
- Possibility of neonatal hypotonia (low muscle tone)
- Frequent respiratory infections are possible
- Life expectancy may be shortened
- Motor milestones will be delayed
- Scoliosis often develops
- Joint contractures
- Fine tremors of the upper extremities[iii]
SMA Type III
Also known as juvenile SMA, this type is a milder form of SMA that starts at a later age than SMA types I and II. Symptoms may begin as early as one year old, most children with SMA type III are diagnosed between 2 and 12 years of age. Occasionally, this diagnosis is not made until adulthood.
Activities such as running, getting up from the floor, and navigating stairs become progressively more difficult as the child ages. Walking is typically possible after a child receives this diagnosis, although their gait pattern may be affected due to weakness. The prognosis for this condition is often normal.[i]
Symptoms:
- Weakness may be noted in youth or even adulthood
- Symptoms are much more variable than SMA type I or II
- Motor difficulties are usually progressive, but may be marked by periods of stability
X-Linked Spinal Bulbar Muscular Atrophy (SBMA)
Also known as Kennedy Disease, x-linked spinal bulbar atrophy is a rare disorder that primarily affects men. Symptom onset can range from the late teens to middle aged, and it preferentially affects the motor neurons that control muscles of the tongue and throat, resulting in chewing and swallowing difficulties. Additionally, individuals with this condition experience varying degrees of muscle weakness, particularly of their facial muscles.
SBMA is caused by a genetic mutation in the androgen receptor gene, and as a result, men affected may exhibit symptoms of androgen deficiency such as breast development, testicular atrophy, reduced libido, impotence, and infertility. Life expectancy is not affected by this condition, although muscle weakness is slowly progressive.[i]
Spinal Muscular Atrophy Physiotherapy
Physiotherapy treatment for SMA will depend on the subtype and the symptoms that are present. Physiotherapy for SMA type I will focus on respiratory techniques to assist with clearing the airways and managing secretions, as well as preventing contractures to allow for hygiene and dressing. Physiotherapy for less involved subtypes such as SMA types II and III will focus more on strengthening, stretching, and functional goals such as independent sitting and walking. As SMA is a lifelong and progressive condition, these individuals will require physiotherapy for long periods of time as they are experiencing a progression of the disease, or working toward a specific functional goal.
Physiotherapy treatment techniques for SMA can include:
- Assessment of baseline range of motion and strength to monitor the progression of the condition
- Prescription of orthotics to improve biomechanical alignment and gait efficiency
- Stretching and mobilization to prevent contractures
- Strengthening exercises to slow muscle deterioration
- Gait and postural control training
- Functional training for daily activities
- Assistance for engagement in meaningful extracurricular activities and sports
- Gait aid prescription and training (walkers, canes, wheelchairs)
- Energy conservation strategies
- Chest physio techniques for client with respiratory involvement[i]
- Airway clearance with cough assist
- Suctioning to clear secretions
- High frequency chest wall oscillation (vest)
- Non-invasive positive pressure ventilation
- Continuous positive airway pressure
Other Spinal Muscular Atrophy Treatment
In addition to physiotherapy treatment, other types of therapy and medical interventions are currently used or being tested for use as effective means of treating symptoms of SMA, including:
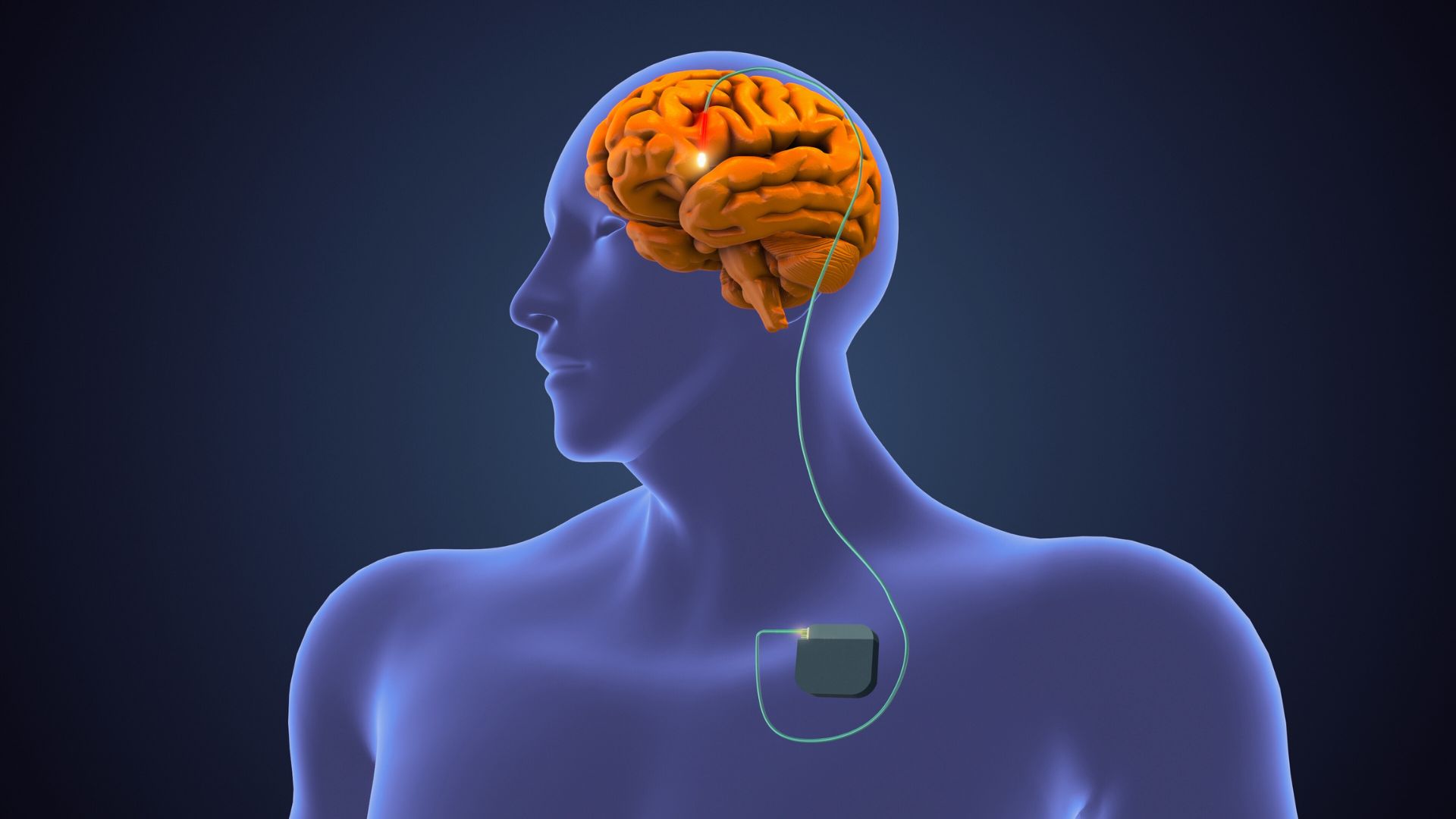
- Medical management – neuroprotective drugs (such as riluzole), medications to improve energy metabolism, and drugs affecting the gene expression of SMA[iii]
- Gene therapy – using viral vectors to replace the SMN 1 gene[iii]
- Stem cell therapy – currently in the testing stages[iii]
- Splinting – for functional use and to prevent contractures
- Speech language pathology for speaking and swallowing difficulties
- Occupational therapy – splinting, seating, feeding issues, adaptive equipment
- Social worker or counsellor to support the client and their family
The clinicians at Propel Physiotherapy have extensive experience treating individuals with neurological conditions. If you have questions about physiotherapy treatment for spinal muscular atrophy, please reach out to us at info@propelphysiotherapy.com or 416-621-2506 to schedule a complimentary consultation with one of our clinicians.
References
[i] Spinal Muscular Atrophy (SMA), Muscular Dystrophy Canada
[ii] Darras BT, Markowitz JA, Monani UR, De Vivo DC. Chapter 8—Spinal Muscular Atrophies. Neuromuscular Disorders of Infancy, Childhood, and Adolescence (Second Edition). San Diego: Academic Press; 2015. p. 117–45
Written by