A sudden twist on the soccer field. A deep squat in the gym that feels a little off. Or maybe just the slow, creeping stiffness that appears one morning when you get out of bed. However, it arrives, knee pain is a signal you can’t ignore—and a meniscus injury is often the culprit.
For years, the standard response to a torn meniscus was surgery. But what if we told you that for many, the most critical tool for a full recovery isn’t a scalpel, but a structured, physiotherapist-guided meniscus injury treatment program?
Whether your injury is a sudden tear from sports or a gradual, age-related degeneration, effective meniscus injury treatment hinges on one thing: restoring your knee’s strength, stability, and function. This guide will walk you through exactly how physiotherapy makes that possible. We’ll explore the causes of meniscus injuries, the symptoms to watch for, and the pivotal role physiotherapy plays in not just healing your knee, but building it back stronger and more resilient than before.
Your journey back to pain-free movement starts here.
Table of Contents
- Understanding the Meniscus
- Common Causes of Meniscus Injuries
- Meniscus Injury Symptoms
- Meniscus Injury Physiotherapy Management
- Phases of Physiotherapy in Meniscus Recovery
- Meniscus Injury Treatment Case Study
- Conclusion
Understanding the Meniscus
Understanding the structure and function of the meniscus is essential before exploring meniscus injury treatment options. Knowing what it is and why it plays such a crucial role in knee health lays the foundation for effective recovery.
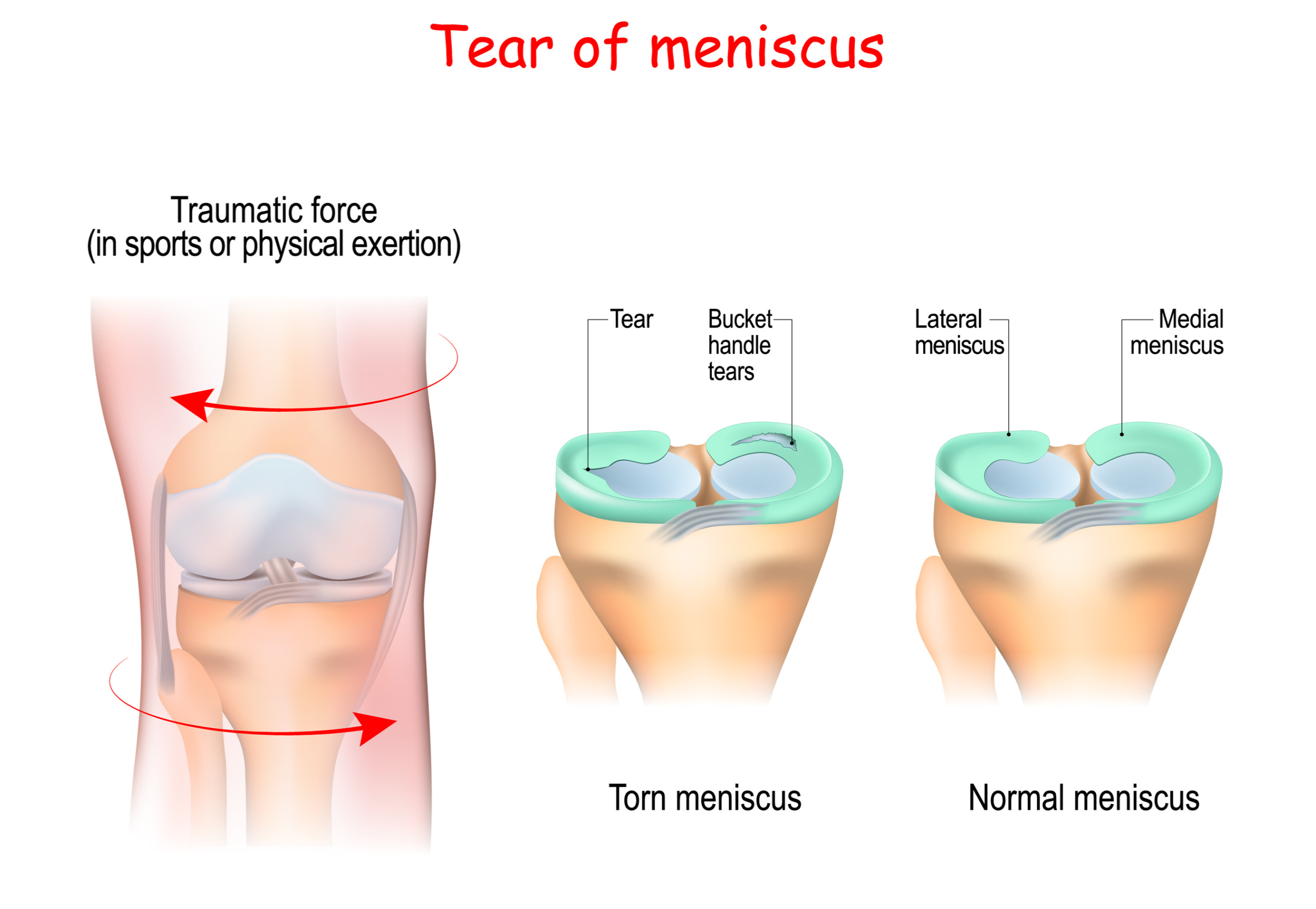
The meniscus is a C-shaped cartilage located in each knee joint that acts like a cushion between your femur (thigh bone) and tibia (shin bone). You have two in each knee — the medial and lateral meniscus. Their job? Absorb shock, stabilize the joint, and help distribute body weight during movement.
Despite its resilience, the meniscus is still vulnerable to injury — especially during twisting movements or deep squats. This is particularly true in sports like football, basketball, tennis, or skiing. Even simple movements like getting up too quickly from a squat can tear the meniscus if it’s already weakened by age or overuse.
Common Causes of Meniscus Injuries
Meniscus injuries are surprisingly common and can affect people of all ages — from athletes in peak condition to older adults performing everyday activities. These injuries result from either sudden trauma or gradual degeneration. Recognizing the underlying causes is essential for both prevention and effective treatment.
1. Sports and High Impact Activities
Athletes, especially those involved in contact sports or sports with quick directional changes, are at higher risk. Movements like pivoting, twisting, jumping, and sudden stops can overload or twist the knee joint, leading to a tear. High-risk sports include: football, soccer, basketball, tennis, and skiing.
2. Trauma or Accidents
A direct blow to the knee — such as a fall, a car accident, or a hit during a game — can compress or twist the knee in ways that damage the meniscus. Examples include: falling on a bent knee, being tackled in sport, and slipping and twisting the knee.
3. Age-Related Degeneration
As we age, our cartilage naturally begins to wear down. For many people over 40, meniscus tears occur without any clear traumatic event. These degenerative tears happen because the cartilage becomes thinner, drier, and less flexible. Risk factors for degenerative tears include: osteoarthritis, long-term repetitive knee strain (e.g., kneeling, climbing stairs), and reduced joint hydration and elasticity with age.
Meniscus injuries aren’t always the result of a single traumatic event — they often develop over time due to repetitive strain or poor movement patterns. Jobs that involve frequent kneeling, squatting, or lifting can place ongoing stress on the knee joint. Similarly, muscle imbalances, weak core or hip muscles, and improper joint alignment can cause the knee to move inefficiently, increasing the risk of injury through everyday motions.
Meniscus Injury Symptoms
Meniscus injuries often present a mix of subtle and obvious symptoms. One of the most common signs is pain along the knee joint, particularly during twisting, squatting, or climbing stairs. The pain may be sharp or dull, and it’s typically located on either the inner (medial) or outer (lateral) side of the knee, depending on where the tear occurred.
Swelling and stiffness are also common. Swelling might appear within hours of an acute injury, or gradually in the case of a degenerative tear. Stiffness can make it hard to fully bend or straighten the knee, often accompanied by a feeling of tightness or fullness in the joint.
A classic sign of a more serious tear is locking or catching of the knee. This happens when a fragment of torn meniscus interferes with joint movement, making it feel like your knee is stuck. You may hear or feel clicking, popping, or grinding during motion.
Some people experience a limited range of motion or a sense of instability, where the knee feels like it might “give out” during walking or turning. This can make daily activities difficult and increases the risk of further injury if left unaddressed.
In older adults, or those with wear-and-tear injuries, symptoms may develop more gradually. These degenerative tears typically cause mild but persistent discomfort, intermittent swelling, and stiffness after activity. Often, there is no clear injury event — just a knee that no longer moves or feels the way it used to.
Meniscus Injury Treatment: Physiotherapy Management
Physiotherapy is a key component in the effective recovery from a meniscus injury because it addresses not just the injury itself, but the overall function and stability of the knee. After a meniscus tear—whether managed surgically or non-surgically—the joint often becomes stiff, weak, and unstable.
Physiotherapy helps restore range of motion, build muscle strength around the knee, and improve balance and coordination. This is critical for reducing pain, preventing further injury, and ensuring a safe return to daily activities or sports.
Physiotherapists tailor treatment plans to individual needs, ensuring a safe and structured path to recovery. They focus on several key areas: reducing pain and swelling, restoring full range of motion, strengthening the muscles that support the knee (especially the quadriceps and hamstrings), and improving balance and coordination. These exercises also help re-train the body to move correctly, reducing the risk of future injuries.
Phases of Physiotherapy in Meniscus Recovery
Rehabilitation for a meniscus injury typically progresses through four key phases, each with specific goals and treatment strategies. Whether the injury is managed surgically or non-surgically, following these phases helps ensure a safe and complete return to function.
| Phase | Timeframe | Focus Area | Activity Examples |
| Acute | 0-2 Weeks | Pain reduction & Protection | RICE, gentle ROM, Isometrics |
| Subacute | 2-6 Weeks | Strength, ROM, Weightbearing | Stationary bike, balance |
| Strength & Control | 6-12 Weeks | Muscle building, Neuromuscular control | Functional movements, squat |
| Return to Activity | 12+ Weeks | Performance, confidence | Agility and plyometrics |
Meniscus Injury Treatment Case Study
The following meniscus injury treatment case study is based on a real client whose name has been altered for privacy.
Patient Profile
- Name: Sarah Manley
- Age: 32
- Occupation: Recreational runner and office worker
- Injury: Medial meniscus tear in the right knee
Background
Sarah Manley experienced a sharp pain in her right knee during a local 10K run. An MRI confirmed a medial meniscus tear. Her orthopedic specialist recommended starting with conservative treatment, and she was referred to physiotherapy.
Physiotherapy Treatment Plan
Our structured rehabilitation plan was divided into 3 progressive phases:
Phase 1: Pain and Swelling Management (Weeks 1–2)
Goals: Reduce inflammation, protect the joint, maintain basic mobility
Key Interventions:
- Rest from aggravating activities (no running or squatting)
- Ice therapy 3–4x daily
- Compression sleeve and elevation
- Education on safe weight-bearing and avoiding twisting motions
Example Exercises:
- Heel Slides – to improve range of motion
- Quad Sets – isometric contraction of quadriceps
- Straight Leg Raises – strengthens without stressing the knee
- Ankle Pumps – to support circulation and reduce swelling
Phase 2: Strength and Mobility (Weeks 3–6)
Goals: Restore range of motion, rebuild muscle strength, improve balance
Key Interventions:
- Begin full weight-bearing as tolerated
- Introduce resistance-based and closed-chain exercises
- Improve joint control and proprioception
Example Exercises:
- Mini Squats (to chair or wall)
- Terminal Knee Extensions with resistance band
- Bridges – to activate glutes and hamstrings
- Single-Leg Balance Drills on foam pad or firm surface
- Stationary Bike – low resistance, no incline
Phase 3: Return to Activity (Weeks 7–10)
Goals: Return to pain-free function, prepare for sport/activity, prevent recurrence
Key Interventions:
- Sport-specific loading and dynamic movement
- Gradual reintroduction of running
- Jump training and lateral movement drills
- Education on long-term joint care
Example Exercises:
- Step-Ups/Step-Downs – increasing step height over time
- Lateral Band Walks – for hip and knee control
- Jog-Walk Intervals – gradual return to running
- Box Jumps or Lunge-to-Balance drills
- Agility Ladder Drills – for coordination and directional control
Outcome
By Week 10, Sarah had returned to running without pain. She regained full knee function and stability, and she was educated on managing training load to prevent re-injury. No surgery was necessary.
Conclusion
Physiotherapy is a key part of successful meniscus injury recovery. It does more than treat symptoms—it helps restore strength, mobility, and stability in the knee, setting the foundation for long-term joint health. Whether you’ve had surgery or are managing the injury conservatively, physiotherapy provides a structured path to healing that’s tailored to your needs and goals.
Physiotherapy guides recovery through each stage—from reducing pain and restoring mobility to rebuilding strength and improving joint stability. A structured rehab plan helps patients recover more efficiently and lowers the risk of reinjury. In many cases, it can even reduce the need for surgery or enhance results after a surgical procedure.
Ultimately, physiotherapy isn’t just a part of the process—it’s a key factor in long-term success. Starting treatment with a physiotherapist early can lead to better movement, faster healing, and a more confident return to your normal activities.
References
Beaufils, P., Becker, R., Kopf, S., Matthieu, O., & Pujol, N. (2017). The knee meniscus: management of traumatic tears and degenerative lesions. EFORT open reviews, 2(5), 195–203. https://doi.org/10.1302/2058-5241.2.160056
Written by