Shin splints, also known as medial tibial stress syndrome (MTSS), are a common exercise-induced condition that affects the lower leg. It is one of the most common running-related musculoskeletal injuries. Studies report incidence rates ranging from 13.6 to 20%, and a prevalence rate of 9.5%.[i]
In this article, we describe the structure and function of the areas affected by shin splints. We also discuss the main causes, signs and symptoms associated with this condition, and common treatment options.
Learn how a shin splints physiotherapy program can help to address the physical impairments and activity limitations from orthopedic injury.
What are Shin Splints?
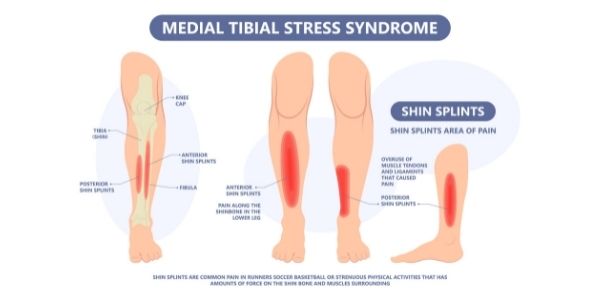
Shin splints refer to exercise-induced leg pain that usually occurs in the middle or bottom third on the inside of the shin. The pain may be tender to touch or can occur as an ache when exercising.
In the acute stages, symptoms are present at the start of activity/exercise but subsides with continued activity. In the subacute stage, it can continue to be present during the activity. In the chronic or later stages, the pain can be present following the completion of activity and can also affect activities of daily living.[ii]
Anatomy and Physiology of the Shin
There are two main bony structures in the lower leg: the tibia (the innermost and larger bone) and the fibula (the outer and smaller bone). The tibia and fibula are covered by the periosteum, which is a thin layer of cells that serves as a transition from the bone and the overlying soft tissue. It also contains cells that help with bone growth and repair.[iii]
While there are many muscles that attach to these structures, the most relevant muscles are the tibialis posterior, the soleus, and the flexor digitorum longus. They have attachments to the rear and innermost part of the tibia, which coincides with the location of shin splints symptoms.
The function of each muscle is listed below:[iii]
- Tibialis posterior: turns the foot inwards, helps with downwards motion.
- Soleus: downwards motion of the foot.
- Flexor Digitorum Longus: bending the big toe downwards, helps with downwards motion of the foot.
Shin Splints Causes
There are several ideas on the cause of shin splints in the literature, with the main explanations involving friction of the periosteum against the surrounding muscles, and/or repetitive stress on the tibia.[iv] Additionally, it is an exercise-induced injury, as symptoms often present at the start of activity or with a sudden increase in exercise intensity.
Some authors suggest that shin splints arise from the repetitive stress of the muscles that attach to the bone.[v] As the tension on the tendons of these muscles increase, it also causes increased strain in the tibial periosteum, which can lead to symptoms.
Another explanation is that repeated weight bearing activities (such as running), causes strain and bending of the tibia. Normally, this leads to bone adaptation to resist tibial bending/strain. When this damage exceeds a threshold and becomes overloaded, it can lead to damage where the bending forces are the greatest.[vi]
Shin Splints Signs and Symptoms
With shin splints, the following signs and symptoms are observed[vii]
- Widespread pain (>5 centimetres) on the inner part of the lower leg or the front of the shin
- Mild swelling of the tibia (shin bone)
Additionally, the following risk factors have been identified for shin splints:[viii]
- Overpronation upon standing or running
- Decreased calf size leading to reduced shock-absorption
- Higher body mass index
- Females
- Below-average activity history
- Previous history of shin splints
- Sudden increase in duration, frequency or intensity of exercise
Shin Splints Treatment
The first line of treatment is typically conservative management with a focus on reduction of symptoms and correction of any biomechanical, muscular or gait causes.
Evidence suggests a graded and conservative approach to the initial treatment of shin splints to be an effective approach:[ix]
- Acute phase: Relative rest or cessation of sport for a prolonged period of time (2-6 weeks).
- Subacute phase: This phase should be focused on modifying activities and training routines. Activity modification may include the reduction of running distance, frequency or intensity by at least 50%. It is also recommended to avoid running on hills, uneven surfaces, or very firm surfaces to reduce strain on the lower extremities.
At this stage, symptoms may also be addressed by changing footwear or obtaining orthotics. This can help to improve shock-absorption during gait and address the alignment of the foot.
In a physiotherapy program, a number of components will be addressed:
- Pain management techniques: This can include modalities such as ultrasound, shock wave therapy and ultrasound, as well as treatment such as soft tissue mobilization and taping.
- Stretching and strengthening exercises: This will help to improve the endurance of the calf musculature and overpronation of gait. Additionally, your provider may also address the strength of the hip and core musculature to improve running mechanics and prevent other overuse injuries.
- Proprioceptive & balance training: This will help to increase the efficiency and the reaction of the leg muscles to react to different running surfaces.
- Cross-training with other low-impact activities: Such activities include pool running, cycling, swimming, or the use of an elliptical machine.
The majority of shin splints cases have significant improvements with conservative management. In cases where individuals do not respond to conservative management, surgical intervention may be indicated.[x] Most surgical procedures involve the reduction of traction on the periosteum.[ix,x]
At Propel Physiotherapy, our team of clinicians can help develop a shin splints physiotherapy program to address physical impairments and activity limitations as a result of this orthopedic injury. We will work with you to achieve your goals get you back to doing what you love.
References
[i] Lopes AD, Hespanhol LC, Yeung SS, Costa LO. What are the main running-related musculoskeletal injuries?. Sports medicine. 2012 Oct;42(10):891-905.
[ii] Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome. Sports medicine. 2009 Jul;39(7):523-46.
[iii] Allen MR, Hock JM, Burr DB. Periosteum: biology, regulation, and response to osteoporosis therapies. Bone. 2004 Nov 1;35(5):1003-12.
[iv] Saxena A, O’Brien T, Bunce D. Anatomic dissection of the tibialis posterior muscle and its correlation to medial tibial stress syndrome. The Journal of foot surgery. 1990 Mar 1;29(2):105-8.
[v] Bouché RT, Johnson CH. Medial tibial stress syndrome (Tibial fasciitis) A proposed pathomechanical model involving fascial traction. Journal of the American Podiatric Medical Association. 2007 Jan;97(1):31-6.
[vi] Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome. Sports medicine. 2009 Jul;39(7):523-46.
[vii] ibid
[viii] Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Current reviews in musculoskeletal medicine. 2009 Sep;2(3):127-33.
[ix] KJ, Engebretsen L, Grøntvedt T, Rossvoll I, Hammer S, Stoltz V. Surgical treatment of medial tibial stress syndrome (shin splint) by fasciotomy of the superficial posterior compartment of the leg. Scandinavian journal of medicine & science in sports. 1995 Feb;5(1):40-3
[x] Winters M, Eskes M, Weir A, Moen MH, Backx FJ, Bakker EW. Treatment of medial tibial stress syndrome: a systematic review. Sports Medicine. 2013 Dec;43(12):1315-33.
Written by